US20040024309A1 - System for monitoring the position of a medical instrument with respect to a patient's body - Google Patents
System for monitoring the position of a medical instrument with respect to a patient's body Download PDFInfo
- Publication number
- US20040024309A1 US20040024309A1 US10/427,472 US42747203A US2004024309A1 US 20040024309 A1 US20040024309 A1 US 20040024309A1 US 42747203 A US42747203 A US 42747203A US 2004024309 A1 US2004024309 A1 US 2004024309A1
- Authority
- US
- United States
- Prior art keywords
- signal
- reference unit
- sensor
- field
- respect
- Prior art date
- Legal status (The legal status is an assumption and is not a legal conclusion. Google has not performed a legal analysis and makes no representation as to the accuracy of the status listed.)
- Abandoned
Links
- 238000012544 monitoring process Methods 0.000 title claims abstract description 13
- 238000001514 detection method Methods 0.000 claims description 41
- 230000005672 electromagnetic field Effects 0.000 claims description 16
- 239000012858 resilient material Substances 0.000 claims 2
- 238000004891 communication Methods 0.000 abstract description 11
- 238000000034 method Methods 0.000 description 17
- 230000005291 magnetic effect Effects 0.000 description 14
- 239000011159 matrix material Substances 0.000 description 8
- 238000013507 mapping Methods 0.000 description 7
- 239000003550 marker Substances 0.000 description 7
- 239000000835 fiber Substances 0.000 description 5
- 230000009466 transformation Effects 0.000 description 5
- 238000003860 storage Methods 0.000 description 4
- 238000001356 surgical procedure Methods 0.000 description 4
- 238000004364 calculation method Methods 0.000 description 3
- 230000005294 ferromagnetic effect Effects 0.000 description 3
- 238000002595 magnetic resonance imaging Methods 0.000 description 3
- 230000003287 optical effect Effects 0.000 description 3
- 238000004458 analytical method Methods 0.000 description 2
- 238000012545 processing Methods 0.000 description 2
- 238000003325 tomography Methods 0.000 description 2
- 230000000007 visual effect Effects 0.000 description 2
- 239000011165 3D composite Substances 0.000 description 1
- 230000005355 Hall effect Effects 0.000 description 1
- 239000000853 adhesive Substances 0.000 description 1
- 230000001070 adhesive effect Effects 0.000 description 1
- 238000013459 approach Methods 0.000 description 1
- 230000005540 biological transmission Effects 0.000 description 1
- 230000001010 compromised effect Effects 0.000 description 1
- 238000012937 correction Methods 0.000 description 1
- 238000002059 diagnostic imaging Methods 0.000 description 1
- 230000000694 effects Effects 0.000 description 1
- 230000005284 excitation Effects 0.000 description 1
- 239000012530 fluid Substances 0.000 description 1
- 238000004519 manufacturing process Methods 0.000 description 1
- 239000000463 material Substances 0.000 description 1
- 238000005259 measurement Methods 0.000 description 1
- 239000002184 metal Substances 0.000 description 1
- 238000012986 modification Methods 0.000 description 1
- 230000004048 modification Effects 0.000 description 1
- 238000005457 optimization Methods 0.000 description 1
- 238000001454 recorded image Methods 0.000 description 1
- 238000004513 sizing Methods 0.000 description 1
- 230000001360 synchronised effect Effects 0.000 description 1
- 238000012795 verification Methods 0.000 description 1
Images
Classifications
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61B—DIAGNOSIS; SURGERY; IDENTIFICATION
- A61B5/00—Measuring for diagnostic purposes; Identification of persons
- A61B5/06—Devices, other than using radiation, for detecting or locating foreign bodies ; determining position of probes within or on the body of the patient
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61B—DIAGNOSIS; SURGERY; IDENTIFICATION
- A61B34/00—Computer-aided surgery; Manipulators or robots specially adapted for use in surgery
- A61B34/20—Surgical navigation systems; Devices for tracking or guiding surgical instruments, e.g. for frameless stereotaxis
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61B—DIAGNOSIS; SURGERY; IDENTIFICATION
- A61B5/00—Measuring for diagnostic purposes; Identification of persons
- A61B5/06—Devices, other than using radiation, for detecting or locating foreign bodies ; determining position of probes within or on the body of the patient
- A61B5/061—Determining position of a probe within the body employing means separate from the probe, e.g. sensing internal probe position employing impedance electrodes on the surface of the body
- A61B5/062—Determining position of a probe within the body employing means separate from the probe, e.g. sensing internal probe position employing impedance electrodes on the surface of the body using magnetic field
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61B—DIAGNOSIS; SURGERY; IDENTIFICATION
- A61B5/00—Measuring for diagnostic purposes; Identification of persons
- A61B5/06—Devices, other than using radiation, for detecting or locating foreign bodies ; determining position of probes within or on the body of the patient
- A61B5/061—Determining position of a probe within the body employing means separate from the probe, e.g. sensing internal probe position employing impedance electrodes on the surface of the body
- A61B5/064—Determining position of a probe within the body employing means separate from the probe, e.g. sensing internal probe position employing impedance electrodes on the surface of the body using markers
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61B—DIAGNOSIS; SURGERY; IDENTIFICATION
- A61B6/00—Apparatus for radiation diagnosis, e.g. combined with radiation therapy equipment
- A61B6/02—Devices for diagnosis sequentially in different planes; Stereoscopic radiation diagnosis
- A61B6/03—Computerised tomographs
- A61B6/032—Transmission computed tomography [CT]
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61B—DIAGNOSIS; SURGERY; IDENTIFICATION
- A61B6/00—Apparatus for radiation diagnosis, e.g. combined with radiation therapy equipment
- A61B6/02—Devices for diagnosis sequentially in different planes; Stereoscopic radiation diagnosis
- A61B6/03—Computerised tomographs
- A61B6/037—Emission tomography
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61B—DIAGNOSIS; SURGERY; IDENTIFICATION
- A61B90/00—Instruments, implements or accessories specially adapted for surgery or diagnosis and not covered by any of the groups A61B1/00 - A61B50/00, e.g. for luxation treatment or for protecting wound edges
- A61B90/10—Instruments, implements or accessories specially adapted for surgery or diagnosis and not covered by any of the groups A61B1/00 - A61B50/00, e.g. for luxation treatment or for protecting wound edges for stereotaxic surgery, e.g. frame-based stereotaxis
- A61B90/14—Fixators for body parts, e.g. skull clamps; Constructional details of fixators, e.g. pins
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61B—DIAGNOSIS; SURGERY; IDENTIFICATION
- A61B90/00—Instruments, implements or accessories specially adapted for surgery or diagnosis and not covered by any of the groups A61B1/00 - A61B50/00, e.g. for luxation treatment or for protecting wound edges
- A61B90/36—Image-producing devices or illumination devices not otherwise provided for
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61B—DIAGNOSIS; SURGERY; IDENTIFICATION
- A61B90/00—Instruments, implements or accessories specially adapted for surgery or diagnosis and not covered by any of the groups A61B1/00 - A61B50/00, e.g. for luxation treatment or for protecting wound edges
- A61B90/39—Markers, e.g. radio-opaque or breast lesions markers
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61B—DIAGNOSIS; SURGERY; IDENTIFICATION
- A61B90/00—Instruments, implements or accessories specially adapted for surgery or diagnosis and not covered by any of the groups A61B1/00 - A61B50/00, e.g. for luxation treatment or for protecting wound edges
- A61B90/90—Identification means for patients or instruments, e.g. tags
- A61B90/98—Identification means for patients or instruments, e.g. tags using electromagnetic means, e.g. transponders
-
- G—PHYSICS
- G01—MEASURING; TESTING
- G01B—MEASURING LENGTH, THICKNESS OR SIMILAR LINEAR DIMENSIONS; MEASURING ANGLES; MEASURING AREAS; MEASURING IRREGULARITIES OF SURFACES OR CONTOURS
- G01B7/00—Measuring arrangements characterised by the use of electric or magnetic techniques
- G01B7/004—Measuring arrangements characterised by the use of electric or magnetic techniques for measuring coordinates of points
-
- G06T3/14—
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61B—DIAGNOSIS; SURGERY; IDENTIFICATION
- A61B17/00—Surgical instruments, devices or methods, e.g. tourniquets
- A61B2017/00017—Electrical control of surgical instruments
- A61B2017/00022—Sensing or detecting at the treatment site
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61B—DIAGNOSIS; SURGERY; IDENTIFICATION
- A61B17/00—Surgical instruments, devices or methods, e.g. tourniquets
- A61B2017/0046—Surgical instruments, devices or methods, e.g. tourniquets with a releasable handle; with handle and operating part separable
- A61B2017/00464—Surgical instruments, devices or methods, e.g. tourniquets with a releasable handle; with handle and operating part separable for use with different instruments
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61B—DIAGNOSIS; SURGERY; IDENTIFICATION
- A61B17/00—Surgical instruments, devices or methods, e.g. tourniquets
- A61B2017/00477—Coupling
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61B—DIAGNOSIS; SURGERY; IDENTIFICATION
- A61B17/00—Surgical instruments, devices or methods, e.g. tourniquets
- A61B2017/00477—Coupling
- A61B2017/00482—Coupling with a code
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61B—DIAGNOSIS; SURGERY; IDENTIFICATION
- A61B34/00—Computer-aided surgery; Manipulators or robots specially adapted for use in surgery
- A61B34/20—Surgical navigation systems; Devices for tracking or guiding surgical instruments, e.g. for frameless stereotaxis
- A61B2034/2046—Tracking techniques
- A61B2034/2051—Electromagnetic tracking systems
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61B—DIAGNOSIS; SURGERY; IDENTIFICATION
- A61B34/00—Computer-aided surgery; Manipulators or robots specially adapted for use in surgery
- A61B34/20—Surgical navigation systems; Devices for tracking or guiding surgical instruments, e.g. for frameless stereotaxis
- A61B2034/2046—Tracking techniques
- A61B2034/2055—Optical tracking systems
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61B—DIAGNOSIS; SURGERY; IDENTIFICATION
- A61B34/00—Computer-aided surgery; Manipulators or robots specially adapted for use in surgery
- A61B34/20—Surgical navigation systems; Devices for tracking or guiding surgical instruments, e.g. for frameless stereotaxis
- A61B2034/2068—Surgical navigation systems; Devices for tracking or guiding surgical instruments, e.g. for frameless stereotaxis using pointers, e.g. pointers having reference marks for determining coordinates of body points
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61B—DIAGNOSIS; SURGERY; IDENTIFICATION
- A61B34/00—Computer-aided surgery; Manipulators or robots specially adapted for use in surgery
- A61B34/20—Surgical navigation systems; Devices for tracking or guiding surgical instruments, e.g. for frameless stereotaxis
- A61B2034/2072—Reference field transducer attached to an instrument or patient
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61B—DIAGNOSIS; SURGERY; IDENTIFICATION
- A61B90/00—Instruments, implements or accessories specially adapted for surgery or diagnosis and not covered by any of the groups A61B1/00 - A61B50/00, e.g. for luxation treatment or for protecting wound edges
- A61B90/08—Accessories or related features not otherwise provided for
- A61B2090/0818—Redundant systems, e.g. using two independent measuring systems and comparing the signals
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61B—DIAGNOSIS; SURGERY; IDENTIFICATION
- A61B90/00—Instruments, implements or accessories specially adapted for surgery or diagnosis and not covered by any of the groups A61B1/00 - A61B50/00, e.g. for luxation treatment or for protecting wound edges
- A61B90/36—Image-producing devices or illumination devices not otherwise provided for
- A61B2090/363—Use of fiducial points
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61B—DIAGNOSIS; SURGERY; IDENTIFICATION
- A61B90/00—Instruments, implements or accessories specially adapted for surgery or diagnosis and not covered by any of the groups A61B1/00 - A61B50/00, e.g. for luxation treatment or for protecting wound edges
- A61B90/39—Markers, e.g. radio-opaque or breast lesions markers
- A61B2090/3937—Visible markers
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61B—DIAGNOSIS; SURGERY; IDENTIFICATION
- A61B90/00—Instruments, implements or accessories specially adapted for surgery or diagnosis and not covered by any of the groups A61B1/00 - A61B50/00, e.g. for luxation treatment or for protecting wound edges
- A61B90/39—Markers, e.g. radio-opaque or breast lesions markers
- A61B2090/3983—Reference marker arrangements for use with image guided surgery
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61B—DIAGNOSIS; SURGERY; IDENTIFICATION
- A61B90/00—Instruments, implements or accessories specially adapted for surgery or diagnosis and not covered by any of the groups A61B1/00 - A61B50/00, e.g. for luxation treatment or for protecting wound edges
- A61B90/10—Instruments, implements or accessories specially adapted for surgery or diagnosis and not covered by any of the groups A61B1/00 - A61B50/00, e.g. for luxation treatment or for protecting wound edges for stereotaxic surgery, e.g. frame-based stereotaxis
-
- A—HUMAN NECESSITIES
- A61—MEDICAL OR VETERINARY SCIENCE; HYGIENE
- A61B—DIAGNOSIS; SURGERY; IDENTIFICATION
- A61B90/00—Instruments, implements or accessories specially adapted for surgery or diagnosis and not covered by any of the groups A61B1/00 - A61B50/00, e.g. for luxation treatment or for protecting wound edges
- A61B90/36—Image-producing devices or illumination devices not otherwise provided for
- A61B90/361—Image-producing devices, e.g. surgical cameras
Definitions
- the invention relates to computer assisted medical surgery and in particular relates to systems for displaying prerecorded visual images during surgical operations.
- CAT Computerized Axial Tomography
- MRI Magnetic Resonance Imaging
- PET Position Emission Tomography
- Prerecorded images may be displayed during surgical operations to provide the surgeon with illustrative reference mappings of pertinent portions of a patient's body.
- Tracking systems for monitoring the position of a medical instrument have also been developed for use with image display systems. Generally, as the surgeon moves the medical instrument with respect to the patient's body, associated prerecorded images are displayed responsive to the movement of the instrument. Such tracking systems typically involve either the use of a passive articulated arm attached to the medical instrument, optical detection or ultrasonic detection.
- Tracking systems using optical detection have been proposed for monitoring the position of a medical instrument with respect to a reference unit as mentioned in U.S. Pat. No. 5,230,623.
- Such systems require that the reference unit and the instrument both be within the view of the camera. This not only limits the movement of the surgical staff, but also requires that at least a portion of the medical instrument remain outside the patient's body.
- Tracking systems using ultrasonic detection are generally disclosed in U.S. Pat. No. 5,230,623. Such systems, however, are disclosed to be used in a fashion similar to optical detection, i.e., triangulation of transmitted signals.
- the transmitted signals are sent from one or more senders to associated receiver(s), and the distances travelled by the signals are determined from either timing or amplitude changes. Again, the transmission path must remain unobstructed.
- a further shortcoming common to each of the above tracking systems is that the patient must not move during the operation. Although the patient is likely to be generally anesthetized, the patient's body may be inadvertently moved by the surgical staff, or the surgeon may want to move the body for better positioning. If the body is moved after the tracking system has been initialized, then the tracking will be misaligned.
- the invention relates to a system for monitoring the position of a medical instrument with respect to a patient's body and for displaying at least one of a plurality of prerecorded images of the body responsive to the position of the medical instrument.
- the system includes a reference unit, a remote unit, a position characteristic field generator, a field sensor, a position detection unit and an output display.
- the reference unit is secured from movement with respect to at least a portion of the patient's body such that the reference unit is substantially immobile with respect to a target operation site.
- the remote unit is attached to the medical instrument.
- the field generator is associated with one of the reference or remote units and generates a position characteristic field, such as a multiplexed magnetic field, in an area including the target operation site.
- the field sensor is associated with the other of the reference or remote units and is responsive to the presence of the field for producing a sensor output signal representative of the sensed field.
- the position detection unit is in communication with the sensor-output signal and produces position data representative of the position of the remote unit with respect to the reference unit.
- the output display unit is in communication with the position detection unit for displaying at least one of the prerecorded images responsive to the position data.
- the system further may include a registration unit in communication with a storage unit and the position data.
- the storage unit stores the plurality of prerecorded images of the body. Each prerecorded image is representative of a planar region within the body such that the plurality of planar regions represented by the prerecorded images define a first coordinate system.
- the registration unit correlates the position data of a second coordinate system (as defined by the position detection unit) with the plurality of prerecorded images of the first coordinate system, and identifies a desired prerecorded image associated with the position of the remote unit with respect to the patient's body.
- the invention also relates to a reference unit that is attachable to a patient's head, and a medical instrument, such as an aspirating device, that is adapted to removably receive a position detection unit.
- FIG. 1 is a diagrammatic view of a system of an embodiment of the invention
- FIG. 2 is a front view of the headset unit shown in FIG. 1;
- FIG. 3 is a side view of the headset unit shown in FIG. 1 taken along line 3 - 3 of FIG. 2;
- FIG. 4 is a rear view of a portion of the headset shown in FIG. 1 taken along line 4 - 4 of FIG. 3;
- FIG. 5 is an exploded side view of the surgical instrument and remote sensor shown in FIG. 1;
- FIG. 6 is an end view of the assembled surgical instrument and sensor shown in FIG. 1 taken along line 6 - 6 of FIG. 5;
- FIG. 7 is a side view of another embodiment of a surgical instrument and sensor unit of the invention in accordance with an alternative embodiment of the invention.
- FIG. 8 is a side view of the surgical instrument shown in FIG. 7;
- FIG. 9 is an end view of the surgical instrument shown in FIG. 7;
- FIG. 10 is an elevational view of the surgical instrument shown in FIG. 7;
- FIG. 11 is a plan view of a remote sensor unit that is adapted to be used with the surgical instrument shown in FIGS. 7 - 10 ;
- FIG. 12 is a side view of another surgical instrument together with the removable remote sensor unit shown in FIGS. 7 and 11;
- FIG. 13 is a diagrammatic illustration of the system employed to prerecord CT images for use with the system of the invention.
- FIG. 14 is diagrammatic illustration of a manual registration process of the invention.
- FIG. 15 is an elevational view of the components of a fiducial marker system in accordance with an embodiment of the invention.
- FIG. 16 is a plan view of the components of the system of FIG. 15 taken along line 16 - 16 thereof;
- FIG. 17 is a flowchart-of the process of using the fiducial marker system of FIG. 15;
- FIG. 18 is a side view of a headset unit in accordance with another embodiment of the invention.
- FIG. 19 is an end view of the headset unit shown in FIG. 18 taken along line 19 - 19 thereof;
- FIG. 20 is a plan view of a transmitter that is adapted to be used with the headset unit shown in FIG. 18;
- FIG. 21 is a partial view of a portion of the headset shown in FIG. 16 taken along line 21 - 21 thereof;
- FIG. 22 is a flow chart of an automatic registration process of the invention.
- FIG. 23 is a diagrammatic view of the position detection components in accordance with a system of the invention.
- FIGS. 24 and 25 are diagrammatic views of the principles of an error detection calculation process in accordance with an embodiment of the invention.
- FIGS. 26 and 27 are diagrammatic views of the errors detected by the process of FIGS. 24 an 25 ;
- FIG. 28 is a diagrammatic view of another embodiment of the invention.
- FIGS. 29 - 32 are diagrammatic views of further embodiments of systems of the invention.
- a system 10 of the invention includes a headset 12 mounted on a patient 14 , a medical instrument 16 , a control system 18 and a display 20 .
- the control system 18 includes a position-detection unit 22 , a registration unit 24 , and an image storage unit 26 .
- the image storage unit 26 stores sets of prerecorded images such as CAT, MRI or PET scan images. Each set of images may be taken along, for example, coronal, sagittal or axial directions. As shown in FIG. 1, the display 20 shows three images, a coronal image 21 a , a sagittal image 21 b , and an axial image 21 c . Text information may also be displayed as shown at 21 d in FIG. 1.
- the headset 12 includes two ear mounts 28 on side members 30 , and a nose bridge mount 32 on a center member 34 .
- the headset 12 should be made of a resilient plastic such that it may be snugly attached to a patient's head, and may be provided in a variety of sizes.
- a primary objective of the headset is to provide a reference unit that may be easily attached to and removed from a patient's head wherein the headset may be repeatedly reattached in exactly the same place with a high degree of accuracy.
- the side members 30 of the headset 12 may be rotationally attached to one another and the ear mounts 28 may be biased toward one another.
- the center member 34 may be rotatable with respect to the side members 30 and biased toward the ear mounts 28 as well.
- the headset 12 shown in FIGS. 1 - 4 also includes a reference unit 36 connected to the position detection unit 22 via communication lines 38 .
- the reference unit 36 may be releasably attached to the headset 12 by conventional clamp or fastening means.
- the reference unit 36 may include a position characteristic field generator capable of generating a multidirectional field in three dimensions and may involve the use of either electromagnetic or ultrasonic waves.
- the position characteristic field differs from the transmit/receive triangulation system, in part, because it does not rely on the comparison of one transmitted signal with another as does triangulation. This permits the path between the field generator and the remote sensor to be obstructed by materials that do not significantly alter the generated field. For example, the position of the medical instrument could be identified even when the instrument is within the patient's body when the generated field is a magnetic field.
- the reference unit may also include a reference sensor 37 to provide verification of proper system operation.
- the field generator includes three orthogonally disposed magnetic dipoles (e.g., current loops or electromagnets), and the orthogonally disposed magnetic fields generated by each of the three dipoles are mutually distinguishable from one another (e.g., via either phase, frequency, or time division multiplexing).
- the near-field characteristics of the multiplexed magnetic fields may be relied upon for position detection, for example as generally described in U.S. Pat. No. 4,054,881.
- the field generator may be located somewhere other than on the headset and the headset may include two field sensors 36 , 37 . When the distance between the sensors 36 , 37 is known, the second sensor may be used to act as a backup or reference check for monitoring the proper operation of the system. If the sensed fields are inconsistent then an error signal is displayed and/or sounded.
- the headset 12 may be employed in systems based on the triangulation of signals where the reference unit 36 includes one or more signal transmitters and/or one or more signal receivers.
- position detection is achieved by comparing certain characteristics of one transmitted signal with those of a second transmitted signal to determine the relative distances travelled.
- the transmitted signals may be electromagnetic (e.g., radio, laser light or light emitting diodes) or may be ultrasonic. The position of the patient's head with respect to the surgical instrument may thereby be monitored.
- the medical instrument 16 may be an aspirating device adapted to removably receive a remote sensor 40 for detecting, for example, the field generated by the position characteristic field generator.
- the sensor 40 may be held inside the instrument 16 by force fit sizing or through the use of a resilient snap member in the wall opening 42 . Since an aspirating device is commonly used in most surgical operations, incorporating the remote sensor into the aspirating device provides the surgeon with a convenient position detection device that does not clutter the operation site with unnecessary items.
- the instrument 16 may further include a second backup field sensor 41 for system error detection as discussed above with reference to the sensor 37 .
- the remote sensors 40 , 41 are removable from the aspirating device and may be interchangeably inserted into any of a variety of specially adapted surgical instruments.
- the remote sensors 40 , 41 are received through an opening 42 in the proximal end of the instrument 16 , and are connected to the position detection unit 22 via communication lines 44 .
- the sensors 40 , 41 may also each include three orthogonally disposed dipole sensing elements for detecting the presence of the field generated by the field generator.
- the field generator and the sensors each include three orthogonally disposed electrical wire loops.
- the generator produces an alternating current through one generator loop at a time thus generating a time division multiplexed alternating electromagnetic field.
- the sensor loop signals are each processed in synchronous timing with the generator loops to produce outputs responsive to each respective alternating electromagnetic field.
- the distal end of the instrument 16 includes a rigid aspirating tube 46 having a flared tip 48 .
- the position of the tip 48 with respect to the center of the remote sensor 40 is a known constant and may be easily seen by the surgeon during surgery.
- the aspirating tube 46 is in fluid communication with an aspirating catheter 50 through the proximal end of the instrument 16 via internal channel 52 and a connector element 54 .
- the aspirating catheter 50 (shown in FIG. 1) is connected to a vacuum aspirating unit (not shown).
- the position detection unit monitors the position of the medical instrument 16 with respect to the reference unit 36 .
- the registration unit 24 correlates the changes in position of the instrument 16 with the spacial orientation of the stored images.
- images appear on the display 20 responsive to the position of the medical instrument 16 .
- This permits the surgeon to always have available the coronal, sagittal, and axial views associated with the precise location of the tip 48 of the instrument 16 regardless of whether the tip 48 is inside of the patient 14 .
- the field generator is attached to the patient's head, the patient is free to be moved without loss of the tracking capabilities.
- the display 20 may further identify the location of the tip 48 on each of the displayed images as shown at 56 in FIG. 1.
- the orientation of the aspirating tube 46 may also be identified on the displayed images.
- a three dimensional composite image may be displayed based on the prerecorded images.
- FIGS. 7 - 11 another embodiment of a removable remote sensor unit 58 may be used with an aspirating device 60 .
- the sensor unit 58 including two sensors 62 , 64 may be removably attached to the device 60 by first engaging recesses 66 on the unit 58 with fingers 68 on the device 60 .
- a tounge 70 on the unit 58 is then received between hinge posts 72 on the device 60 , and finally secured in place by rotating the lock 74 from an open position as shown in FIG. 8 to a closed position as shown in FIG. 7.
- the lock 74 includes a recessed area at 76 adapted to frictionally engage the tounge 70 on the sensor unit 58 .
- the sensor unit 58 further includes the ability to identify which of a plurality of medical instruments is attached to the sensor unit 58 at any time.
- the unit 58 includes a plurality of Hall effect transistors 78
- the medical instrument 60 includes one or more tiny permanent magnets 80 .
- the transistors 78 identify which of the medical instruments is attached to the sensor unit 58 .
- the instrument 60 shown in FIGS. 7 - 11 is known to be attached to the sensor unit 58 since the instrument 60 includes three magnets. If only two magnets 82 are sensed then the medical instrument attached to the sensor unit 58 is a different instrument 84 as shown in FIG. 12. If no magnets are sensed then it is known that the sensor unit 58 is not attached to any medical instrument. Knowing the identity of the attached medical instrument permits the system to automatically adjust the position detection unit to compensate for the differences in instrument tip position with respect to the position of the sensors 62 , 64 for a variety of medical instruments.
- the removably engageable feature of the sensor unit not only provides versatility, but also facilitates the use of sterilized medical instruments.
- the registration process involves two fundamental steps: 1) recording the scan images of a predetermined orientation and 2) mapping the special orientation of the position detection system onto the recorded images.
- the orientations of the prerecorded images may be in the sagittal (i-j plane), coronal (k-j plane) and/or axial (k-i plane) as shown in FIG. 13.
- the images may be digitally stored and the distance between each scanned image is recorded, as are the relative orientations of each set of images.
- certain of the images may be created from other images without the need to prerecord each of the sagittal, coronal and axial views. For example, by multiplanar reformatting the sagittal and coronal images may be created from the axial images.
- fiducial markers 90 are placed on the patient's head 14 prior to scanning with the scanner 92 .
- the markers then appear on certain of the scanned images, and may be located by the position detection system as shown in FIG. 14. Specifically, when each marker 90 is sequentially located, for example with the tip 48 of a medical instrument 16 , the user locates the same marker on the prerecorded images by using, for example a computer mouse. The user then controls the entering of the registration data through either a computer keyboard 94 , a mouse, or a foot switch.
- the registration unit may scan each prerecorded digital image beginning from one corner until it locates the identified marker.
- fiducial markers 90 ′ may be adhered to intermediate adhesive strips 91 which are directly adhered to the patient's skin 93 as shown in FIGS. 15 and 16.
- the fiducial markers 90 ′ include a radiopaque element 95 and the strips 91 include a small puncture hole or other marker 97 .
- the process of using the fiducial markers 90 ′ begins (step 1700 ) by first placing the strips 91 on the patient's skin (step 1710 ). The fiducial markers 90 ′ are then placed on the strips 91 such that the radiopaque elements 95 align with the markers 97 on the strips 91 (step 1704 ). The scan images are then recorded (step 1706 ), and the fiducial markers 90 ′ may then be removed from the patient (step 1708 ).
- the surgeon or technician may locate the markers 97 with the tip of a pointer (step 1710 ) and thereby record the positions of the fiducial marker radiopaque elements 95 with respect to the transmitter.
- the use of the intermediate strips 91 not only provides increased comfort to the patient after the image scanning and prior to surgery, but also facilitates accurate registration. Since the radiopaque elements 95 were centered directly on top of the markers 93 , the accuracy of registration is enhanced because the user may now locate the smaller sized markers 93 instead of more indefinitely locating a portion of the larger sized radiopaque elements 95 with the pointer tip.
- the registration unit generates, a mapping function to translate the position detection data (in x-y-z coordinates) to the stored image orientation data (in i-j-k coordinates).
- the mapping equation is determined by using Powell's method as follows.
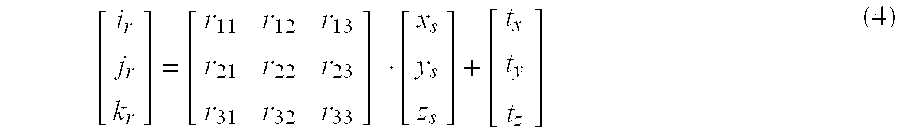
- the images points are each processed as a matrix of the form [ i r j r k r ] ( 1 )
- a computer processor then iteratively calculates the optimal values for the transformation matrices [ r 11 r 12 r 13 r 21 r 22 r 23 r 31 r 32 r 33 ] ⁇ ⁇ and ⁇ [ t x t y t z ] ⁇ ( 3 )
- the optimal values for the transformation matrices comprise the transformation equation and may now be used to translate the position of the medical instrument with respect to the transmitter in the x-y-z coordinate system, to the appropriate orientation of the prerecorded images in the i-j-k coordinate system.
- a further embodiment of the headset of the invention may be employed in an automatic registration process.
- a headset 100 of the invention includes two ear mounts 28 , side members 30 , and a nose bridge mount 32 on center member 34 as discussed above with reference to FIGS. 2 - 4 .
- the headset 100 further includes a center plate 102 on the center member 34 .
- the center plate 102 is adapted to receive a transmitter 104 as shown in phantom in FIG. 19 and shown from the underside of the plate 102 in FIG. 21.
- the transmitter 104 includes two posts 106 and a key 108 that is free to rotate about a pin 110 .
- the key is passed through a longitudinal opening 112 in the plate 102 , and the posts 106 are each received by post openings 114 .
- One of the post openings 114 is preferably formed as a slot to provide a snug fit for the transmitter yet still accommodate variations between headsets due to manufacturing tolerances.
- the key 108 may then be rotated to lock the transmitter onto the outer facing surface of the plate 102 .
- the transmitter 104 may then be removed from and reattached to identical headsets in the same location and orientation with a high degree of accuracy.
- the headset 100 further includes very small (e.g., about 2 mm dia.) metal fiducial balls 116 secured within the center plate 102 as shown in FIG. 18.
- the automatic registration process locates the balls 116 on the prerecorded scan images, and knowing the spacial relationship between the balls 116 and the transmitter 104 , automatically generates the mapping function to translate from the transmitter coordinate system to the image coordinate system.
- the automatic registration process begins (step 2200 ) by loading the prerecorded images (step 2202 ) and then creating a three dimensional data set (step 2204 ). Pixels having an intensity within a certain range are then identified (step 2206 ), and groups of adjacent pixels are located (step 2208 ) and classified together as a single group. The volume of each group is calculated (step 2210 ) and groups not within a predefined range of volumes are rejected (step 2212 ). Groups not having at least one pixel with an intensity level of at least a certain amount are rejected (step 2214 ). If the number of groups remaining is less than the number of fiducial balls 116 (step 2216 ), e.g., 7 , then the program ends having failed to provide automatic registration (steps 2218 and 2220 ).
- the center of each group is then located and the distances between each group's center and the other centers are calculated and recorded in a matrix of at least 7 by 7 (step 2222 ).
- the known distances between the fiducial balls comprise a predefined 7 by 7 matrix.
- the program compares each of the known distances with the various predefined distances between the fiducial balls, then generates a best fit approximation of the correlation between the sets of distances (step 2224 ). If the distance correlation provides an approximation outside of a preset tolerance (step 2226 ) then the program ends (steps 2218 and 2220 ) having failed to automatically generate the transformation matrices.
- step 2228 If the correlation of distances is within tolerance and there are seven groups (step 2228 ) then the image data is, recorded in the image matrix (step 2230 ). If the number of groups is above seven, then a geometry correlation is performed comparing the geometry of the groups to the known geometry of the fiducial balls (step 2232 ). If the geometry correlation is successful (step 2234 ) then the transformation matrices are recorded (step 2230 ), and if not the program reports the error condition (step 2218 ).
- mapping equation may now be automatically generated as discussed above with reference to Powell's method.
- the registration program may automatically locate portions of the reference unit itself on the scanned images, thereby identifying the orientation of the reference unit with respect to the scanned images. Again, since the relative orientation of the field generator with respect to the reference unit is known, the registration unit may then generate the appropriate mapping function.
- the surfaces of the patient's skin may be tracked such as by a laser light pointer or a movable tip pointer that is biased in a forward direction. The tracked surfaces may then be located on the stored images.
- the registration unit could be programmed to identify characteristic structures or features of the patient's body and thereby provide fully automatic registration. For example, the system might, knowing the size and shape of a headset, identify where the headset would be placed on the patient's head, even though it does not appear on the prerecorded images.
- the position detection system may operate by any desired principle suitable for generating a field in which position detection may be achieved at any location within the field.
- any desired principle suitable for generating a field in which position detection may be achieved at any location within the field For example, it has been found that the 3 Spaces FastrakTM product sold by Polhemus, Incorporated of Colchester, Vermont operates via principles suitable for use in the present invention. This product uses three orthogonally disposed magnetic dipoles for both the transmitter and the sensor, and produces alternating electromagnetic fields of 8-14 kHz that are time division multiplexed.
- both the magnetic field source 101 and the magnetic field sensor 103 include three orthogonally disposed coils as shown.
- An alternating electric current from an amplifier 105 is passed through each of the source coils one at a time generating sequential magnetic fields.
- a processing unit 107 generates the timing signals and controls a digital-to-analog converter 109 .
- the magnetic fields induce voltages in the three coils of the sensor 103 .
- the induced voltages are amplified by an amplifier 111 , digitized by an analog-to-digital converter 113 , and then processed by the processing unit 107 .
- the time division multiplexed excitation of the three coils of the source creates a unique magnetic field sequence throughout the field of the source.
- the six degree of freedom data can be calculated from the data present on the three coils of the sensor.
- the six degree of freedom information is then sent to a host computer 115 .
- the position of a sensor S with respect to the field generator defining a reference coordinate frame (X,Y,Z) may be produced by the 3 Space® FastrakTM product at a given time as a set of six values x s , y s , z s , ⁇ azs , ⁇ els , and ⁇ ros .
- the values x s , y s , and z s identify the position of the center of the sensor within the X,Y,Z coordinate reference frame, and the angles ⁇ azs , ⁇ els , and ⁇ ros identify the orientation of the-sensor S with respect to the X,Y,Z coordinate reference frame.
- the value ⁇ azs is the azimuth angle of the sensor.
- the azimuth angle identifies the amount of rotation of the X and Y reference axes together about the Z axis to a new position in which the X axis is aligned with the center of the sensor in the Z direction.
- the new positions of the X and Y axes are defined as X′ and Y′ respectively.
- the value ⁇ els is the elevation angle of the sensor.
- the elevation angle identifies the amount of rotation of the X′ and Z axes together about the Y′ axis to a new position in which the X′ axis is aligned with the center of the sensor S.
- the new positions of the X′ and Z axes are defined as X′′ and Z′ respectively.
- the value ⁇ ros is the roll angle of the sensor.
- the roll angle identifies the amount of rotation of the Y′ and Z′ axes together about the X′′ axis to a new position defining new axes Y′′ and Z′′ respectively.
- the sensor is oriented in the X′′,Y′′,Z′′ reference frame, and this orientation is defined by the values ⁇ azs , ⁇ els , and ⁇ ros .
- the combined power of all the sensor data is inversely proportional to the distance of the sensor from the source.
- the ratio between the sensor data components, created by the individual source coils, will determine the x, y, z position coordinate of the sensor.
- the ratio between the individual sensor coil data will determine the orientation of the sensor.
- the speed of the instrument should be monitored. If the speed of movement of the instrument is above a defined threshold, then inconsistent sensor readings should be ignored until the speed falls below the threshold.
- the speed may be monitored by calculating a weighted sum of the differences between each of the x, y, and z coordinates at successive time intervals t 1 and t 2 .
- a reference sensor 37 may be securely mounted on the transmitter assembly 12 at a fixed distance from the center of the transmitter 36 .
- the location and orientation of this reference sensor should be determined through a calibration process under controlled conditions, and thereafter continuously calculated and verified.
- a weighted sum of all six sensor output parameters x s , y s , Z s , ⁇ azs , ⁇ els , and ⁇ ros may be continuously monitored as an indication of compromised field integrity.
- the remote sensor 58 may include a plurality of sensors ( 62 , 64 ) the outputs of which are compared for error detection purposes.
- Potential error conditions that would be detectable by such a system include sensor failure where one sensor ceases to operate properly, as well as uneven localized field distortions in the area of the medical instrument.
- an error detection system sufficient to identify localized uniform distortions in the area of the medical instrument or headset may be designed using two sensors separated by a fixed distance as shown in FIGS. 7 - 12 and by monitoring the locations of two or more virtual points.
- the sensors S 1 and S 2 are separated from each other by a distance 2d and for convenience defined to be positioned along an axis such as the Y axis as shown.
- Sensor S 1 uniquely defines an X-Z plane in which it is located
- S 2 uniquely defines an X-Z plane in which it is located as shown.
- a first virtual location v a is chosen to be between the X-Z planes defined by the sensors, while a second virtual location v b is chosen to be outside of the X-Z planes defined by the sensors as shown in FIG. 11.
- the locations v a and v b are virtual locations that are continuously calculated and compared with factory defined positions.
- the virtual points v a (-d,-d,-d with respect to S 2 ) and v b (d,d,d with respect to S 2 ) are equidistant from S 2 .
- the sensor S 2 is the protected sensor in this embodiment, and the sensor S 1 is used as a reference to provide the error detection for S 2
- the magnitude of the resultant vector from S 2 to v a is the same as that from S 2 to V b but opposite in direction, and this magnitude is approximately one half of the distance between S 1 and S 2 .
- the locations of v a and V b in the reference coordinate system (i.e., with respect to S 1 ) must be calculated and will be referred to as v a1 and V b1
- the location (PS) and the orientation of the protected sensor (S1) with respect to the reference sensor must be determined.
- the attitude matrix (A) is calculated from the orientation values of the protected sensor: [ cos ⁇ ⁇ ⁇ ? ⁇ cos ⁇ ⁇ ⁇ ? sin ⁇ ⁇ ⁇ ? ⁇ cos ⁇ ⁇ ⁇ ? - sin ⁇ ⁇ ⁇ ? cos ⁇ ⁇ ⁇ ? - sin ⁇ ⁇ ⁇ ? - sin ⁇ ⁇ ⁇ ? - sin ⁇ ⁇ ⁇ ⁇ ? ?
- the operation is based in part on the principle that if the position error is being reduced by the orientation error at one virtual point, then the error will be increased at the other virtual point causing a field integrity violation signal to be generated. If for example, there is an error in the measured position and orientation of the protected sensor, then the measured value will have an error added to the established value.
- the field integrity checking is performed in this case as follows:
- this relationship may be diagrammatically illustrated as shown in FIG. 27.
- the tip location of the medical instrument should be initially defined with respect to the protected sensor (S2), and used in determining the position of the tip with respect to the source.
- the integrity of the field generated by the field generator may be monitored as discussed above by positioning a reference sensor a fixed distance from the generator, and continuously monitoring its position for any changes.
- the calculations involved in the above field integrity detection analysis regarding the two sensors S 1 and S 2 may be performed for a transmitter and single sensor field integrity detection system. Specifically, the calculations may be performed by substituting the field transmitter for the protected sensor (S 2 ), and by substituting the single sensor for the reference sensor (S 1 ). These field integrity analyses may also be used to identify the half field of the operation environment.
- a reference unit 120 including a field generator 122 , may be positioned a small distance away from the portion of the patient's body (such as the head) 14 on an articulated arm 124 .
- a headset 12 including a reference sensor 126 may be attached to the patient's body, and the medical instrument 16 may include a remote sensor 40 as discussed above with reference to FIGS. 1 - 6 .
- the field generator 122 Once the field generator 122 is positioned at a convenient location it may be fixed in place by securing the joints of the articulated arm. The position of the patient with respect to the field generator may accordingly be monitored. The position of the instrument 16 with respect to the patient may also be determined and the system may then operate to display the appropriate prerecorded images as discussed below.
- the position of the field generator 88 may be adjusted during the surgical operation by moving the articulated joints. If neither the remote sensor 40 nor the reference sensor 126 are moved with respect to one another, then moving the field generator 122 should not affect the position detection system. If the accuracy of the system depends at all on the relative positions of the field generators 122 and the sensors 40 , 126 , then it may be desirable to move the field generator 122 during the surgical operation. This may be the case, for example, if the system relies on the near-field characteristics of a multiplexed magnetic field wherein it might be desirable to keep the sensors 40 , 126 generally equidistant from the generator 122 .
- system may periodically prompt the user to reposition the generator 122 such as through visual cues on the display.
- the relative positioning of the field generator and the one or more field sensors is in no way limited to those shown.
- the monitoring of the position of the patient may be accomplished by means other than using a headset and reference sensor.
- a camera 128 connected to an image processor 130 may be positioned to record the location of the field generator with respect to the target operation site of the patient as shown in FIG. 29. If either the patient or the field generator is moved, the image processor 130 will identify the amount of relative change in location and advise the position detection unit 22 accordingly. Additional cameras positioned to view the patient from a variety of directions may be employed in further embodiments.
- the system may include a flexible band 132 for secure attachment to a portion of a patient's body 14 (e.g., a head or chest).
- the band 132 includes field generator 134 and a reference sensor 136 that provides feedback to the signal generator in the position detection unit 22 .
- the position detection unit 22 is connected via communication lines 138 to the flexible band 132 , and is connected via communication lines 140 to a flexible medical instrument 142 having a remote sensor at its tip 144 . Because the medical instrument 142 is not rigid, the sensor should be positioned sufficiently close to the tip of the instrument 142 to provide accurate position detection and monitoring within the patient's body.
- the display 20 may indicate the relative orientation of the instrument 142 on one or more images as shown.
- a system of the invention may include a flexible medical instrument 150 having a sensor 152 at its distal tip 154 , and a fiber optic endoscope 156 having a sensor 158 at it distal tip. 160 .
- the fiber optic endoscope 156 is connected at its proximal end to a camera 162 which is in communication with an image processor 164 . Because the field generator 134 on the reference band 132 may move, for example as the patient breaths, the location of the remote sensor 152 may appear to move when in fact the medical instrument 150 has not moved.
- the fiber optic endoscope 156 can be used to monitor the position of the tip 154 of the instrument 150 with respect to the inside of the patient's body as shown. Any sensed movement of the sensor 152 with respect to the field generator 134 can be evaluated with reference to whether the tip 154 has moved with respect to the interior of the patient's body. If the camera observes that the tip 154 has not moved, but the sensor 152 indicates that it has moved, then the system can identify that such movement was due to the movement of the field generator and not the sensor 152 . The system may then automatically correct for such variation. Further, the fiber optic endoscope 156 itself may include a sensor 158 for detecting whether the tip 160 of the fiber optic has moved. This should further enhance the accuracy of the correction system. Also, the camera 162 may provide continuous registration of the prerecorded images based on the internal structure of the patient's body.
Landscapes
- Health & Medical Sciences (AREA)
- Life Sciences & Earth Sciences (AREA)
- Engineering & Computer Science (AREA)
- Surgery (AREA)
- Medical Informatics (AREA)
- Veterinary Medicine (AREA)
- Biomedical Technology (AREA)
- Heart & Thoracic Surgery (AREA)
- Molecular Biology (AREA)
- Animal Behavior & Ethology (AREA)
- General Health & Medical Sciences (AREA)
- Public Health (AREA)
- Pathology (AREA)
- Physics & Mathematics (AREA)
- Nuclear Medicine, Radiotherapy & Molecular Imaging (AREA)
- Biophysics (AREA)
- Oral & Maxillofacial Surgery (AREA)
- Human Computer Interaction (AREA)
- High Energy & Nuclear Physics (AREA)
- Radiology & Medical Imaging (AREA)
- Optics & Photonics (AREA)
- Pulmonology (AREA)
- Theoretical Computer Science (AREA)
- Robotics (AREA)
- Electromagnetism (AREA)
- Neurosurgery (AREA)
- General Physics & Mathematics (AREA)
- Magnetic Resonance Imaging Apparatus (AREA)
- Measurement Of Length, Angles, Or The Like Using Electric Or Magnetic Means (AREA)
- Apparatus For Radiation Diagnosis (AREA)
- Endoscopes (AREA)
Abstract
Description
- The invention relates to computer assisted medical surgery and in particular relates to systems for displaying prerecorded visual images during surgical operations.
- Presently available medical imaging techniques such as CAT (Computerized Axial Tomography), MRI (Magnetic Resonance Imaging), and PET (Position Emission Tomography), are known to be helpful not only for diagnostic purposes, but also for providing assistance during surgery. Prerecorded images may be displayed during surgical operations to provide the surgeon with illustrative reference mappings of pertinent portions of a patient's body.
- Tracking systems for monitoring the position of a medical instrument have also been developed for use with image display systems. Generally, as the surgeon moves the medical instrument with respect to the patient's body, associated prerecorded images are displayed responsive to the movement of the instrument. Such tracking systems typically involve either the use of a passive articulated arm attached to the medical instrument, optical detection or ultrasonic detection.
- Tracking systems using a passive articulated mechanical arm attached to a medical instrument are disclosed in U.S. Pat. Nos. 5,186,174 and 5,230,623. Generally, as the surgeon moves the surgical instrument with respect to the patient's body, micro recorders at the joints of the articulated arm record the respective amounts of movement of each arm member. The outputs of the micro recorders are processed and the position of the medical instrument with respect to the base of the articulated arm is thereby monitored. One or more prerecorded images are then displayed responsive to the movement of the surgical instrument. Such articulated arm tracking systems, however, require that the instrument be attached to a cumbersome mechanical arm. Also, although free movement of the tip of the arm in three dimensional space may be theoretically possible, the surgeon might experience difficulty positioning the instrument at certain locations and in desired orientations within the body.
- Tracking systems using optical detection (video cameras and/or CCDs (Charge Coupled Devices)) have been proposed for monitoring the position of a medical instrument with respect to a reference unit as mentioned in U.S. Pat. No. 5,230,623. Such systems, however, require that the reference unit and the instrument both be within the view of the camera. This not only limits the movement of the surgical staff, but also requires that at least a portion of the medical instrument remain outside the patient's body.
- Tracking systems using ultrasonic detection are generally disclosed in U.S. Pat. No. 5,230,623. Such systems, however, are disclosed to be used in a fashion similar to optical detection, i.e., triangulation of transmitted signals. The transmitted signals are sent from one or more senders to associated receiver(s), and the distances travelled by the signals are determined from either timing or amplitude changes. Again, the transmission path must remain unobstructed.
- A further shortcoming common to each of the above tracking systems is that the patient must not move during the operation. Although the patient is likely to be generally anesthetized, the patient's body may be inadvertently moved by the surgical staff, or the surgeon may want to move the body for better positioning. If the body is moved after the tracking system has been initialized, then the tracking will be misaligned.
- There is a need therefore for a system for monitoring the position of a medical instrument with respect to a patient's body that avoids these and other shortcomings of present devices.
- The invention relates to a system for monitoring the position of a medical instrument with respect to a patient's body and for displaying at least one of a plurality of prerecorded images of the body responsive to the position of the medical instrument. The system includes a reference unit, a remote unit, a position characteristic field generator, a field sensor, a position detection unit and an output display.
- In one embodiment, the reference unit is secured from movement with respect to at least a portion of the patient's body such that the reference unit is substantially immobile with respect to a target operation site. The remote unit is attached to the medical instrument. The field generator is associated with one of the reference or remote units and generates a position characteristic field, such as a multiplexed magnetic field, in an area including the target operation site. The field sensor is associated with the other of the reference or remote units and is responsive to the presence of the field for producing a sensor output signal representative of the sensed field.
- The position detection unit is in communication with the sensor-output signal and produces position data representative of the position of the remote unit with respect to the reference unit. The output display unit is in communication with the position detection unit for displaying at least one of the prerecorded images responsive to the position data.
- The system further may include a registration unit in communication with a storage unit and the position data. The storage unit stores the plurality of prerecorded images of the body. Each prerecorded image is representative of a planar region within the body such that the plurality of planar regions represented by the prerecorded images define a first coordinate system. The registration unit correlates the position data of a second coordinate system (as defined by the position detection unit) with the plurality of prerecorded images of the first coordinate system, and identifies a desired prerecorded image associated with the position of the remote unit with respect to the patient's body.
- The invention also relates to a reference unit that is attachable to a patient's head, and a medical instrument, such as an aspirating device, that is adapted to removably receive a position detection unit.
- The following detailed description of the invention may be further understood with reference to the accompanying drawings in which: FIG. 1 is a diagrammatic view of a system of an embodiment of the invention;
- FIG. 2 is a front view of the headset unit shown in FIG. 1;
- FIG. 3 is a side view of the headset unit shown in FIG. 1 taken along line 3-3 of FIG. 2;
- FIG. 4 is a rear view of a portion of the headset shown in FIG. 1 taken along line 4-4 of FIG. 3;
- FIG. 5 is an exploded side view of the surgical instrument and remote sensor shown in FIG. 1;
- FIG. 6 is an end view of the assembled surgical instrument and sensor shown in FIG. 1 taken along line 6-6 of FIG. 5;
- FIG. 7 is a side view of another embodiment of a surgical instrument and sensor unit of the invention in accordance with an alternative embodiment of the invention;
- FIG. 8 is a side view of the surgical instrument shown in FIG. 7;
- FIG. 9 is an end view of the surgical instrument shown in FIG. 7;
- FIG. 10 is an elevational view of the surgical instrument shown in FIG. 7;
- FIG. 11 is a plan view of a remote sensor unit that is adapted to be used with the surgical instrument shown in FIGS. 7-10;
- FIG. 12 is a side view of another surgical instrument together with the removable remote sensor unit shown in FIGS. 7 and 11;
- FIG. 13 is a diagrammatic illustration of the system employed to prerecord CT images for use with the system of the invention;
- FIG. 14 is diagrammatic illustration of a manual registration process of the invention;
- FIG. 15 is an elevational view of the components of a fiducial marker system in accordance with an embodiment of the invention;
- FIG. 16 is a plan view of the components of the system of FIG. 15 taken along line 16-16 thereof;
- FIG. 17 is a flowchart-of the process of using the fiducial marker system of FIG. 15;
- FIG. 18 is a side view of a headset unit in accordance with another embodiment of the invention;
- FIG. 19 is an end view of the headset unit shown in FIG. 18 taken along line 19-19 thereof;
- FIG. 20 is a plan view of a transmitter that is adapted to be used with the headset unit shown in FIG. 18;
- FIG. 21 is a partial view of a portion of the headset shown in FIG. 16 taken along line 21-21 thereof;
- FIG. 22 is a flow chart of an automatic registration process of the invention;
- FIG. 23 is a diagrammatic view of the position detection components in accordance with a system of the invention;
- FIGS. 24 and 25 are diagrammatic views of the principles of an error detection calculation process in accordance with an embodiment of the invention;
- FIGS. 26 and 27 are diagrammatic views of the errors detected by the process of FIGS. 24 an 25;
- FIG. 28 is a diagrammatic view of another embodiment of the invention; and
- FIGS. 29-32 are diagrammatic views of further embodiments of systems of the invention.
- As shown in FIG. 1, a system 10 of the invention includes a
headset 12 mounted on apatient 14, amedical instrument 16, acontrol system 18 and adisplay 20. Thecontrol system 18 includes a position-detection unit 22, aregistration unit 24, and animage storage unit 26. - The
image storage unit 26 stores sets of prerecorded images such as CAT, MRI or PET scan images. Each set of images may be taken along, for example, coronal, sagittal or axial directions. As shown in FIG. 1, thedisplay 20 shows three images, acoronal image 21 a, asagittal image 21 b, and anaxial image 21 c. Text information may also be displayed as shown at 21 d in FIG. 1. - As further shown in FIGS. 2-4, the
headset 12 includes two ear mounts 28 onside members 30, and anose bridge mount 32 on acenter member 34. Theheadset 12 should be made of a resilient plastic such that it may be snugly attached to a patient's head, and may be provided in a variety of sizes. A primary objective of the headset is to provide a reference unit that may be easily attached to and removed from a patient's head wherein the headset may be repeatedly reattached in exactly the same place with a high degree of accuracy. In other embodiments, theside members 30 of theheadset 12 may be rotationally attached to one another and the ear mounts 28 may be biased toward one another. Further, thecenter member 34 may be rotatable with respect to theside members 30 and biased toward the ear mounts 28 as well. - The
headset 12 shown in FIGS. 1-4 also includes areference unit 36 connected to theposition detection unit 22 via communication lines 38. Thereference unit 36 may be releasably attached to theheadset 12 by conventional clamp or fastening means. In one embodiment thereference unit 36 may include a position characteristic field generator capable of generating a multidirectional field in three dimensions and may involve the use of either electromagnetic or ultrasonic waves. The position characteristic field differs from the transmit/receive triangulation system, in part, because it does not rely on the comparison of one transmitted signal with another as does triangulation. This permits the path between the field generator and the remote sensor to be obstructed by materials that do not significantly alter the generated field. For example, the position of the medical instrument could be identified even when the instrument is within the patient's body when the generated field is a magnetic field. Additionally, the reference unit may also include areference sensor 37 to provide verification of proper system operation. - In the present embodiment the field generator includes three orthogonally disposed magnetic dipoles (e.g., current loops or electromagnets), and the orthogonally disposed magnetic fields generated by each of the three dipoles are mutually distinguishable from one another (e.g., via either phase, frequency, or time division multiplexing). The near-field characteristics of the multiplexed magnetic fields may be relied upon for position detection, for example as generally described in U.S. Pat. No. 4,054,881. In alternate embodiments the field generator may be located somewhere other than on the headset and the headset may include two
field sensors sensors - In other embodiments the
headset 12 may be employed in systems based on the triangulation of signals where thereference unit 36 includes one or more signal transmitters and/or one or more signal receivers. In such a triangulation system, position detection is achieved by comparing certain characteristics of one transmitted signal with those of a second transmitted signal to determine the relative distances travelled. The transmitted signals may be electromagnetic (e.g., radio, laser light or light emitting diodes) or may be ultrasonic. The position of the patient's head with respect to the surgical instrument may thereby be monitored. - As shown in FIGS. 5 and 6 the
medical instrument 16 may be an aspirating device adapted to removably receive aremote sensor 40 for detecting, for example, the field generated by the position characteristic field generator. Thesensor 40 may be held inside theinstrument 16 by force fit sizing or through the use of a resilient snap member in thewall opening 42. Since an aspirating device is commonly used in most surgical operations, incorporating the remote sensor into the aspirating device provides the surgeon with a convenient position detection device that does not clutter the operation site with unnecessary items. Theinstrument 16 may further include a secondbackup field sensor 41 for system error detection as discussed above with reference to thesensor 37. - The
remote sensors remote sensors opening 42 in the proximal end of theinstrument 16, and are connected to theposition detection unit 22 via communication lines 44. Thesensors - The distal end of the
instrument 16 includes arigid aspirating tube 46 having a flaredtip 48. The position of thetip 48 with respect to the center of theremote sensor 40 is a known constant and may be easily seen by the surgeon during surgery. The aspiratingtube 46 is in fluid communication with an aspiratingcatheter 50 through the proximal end of theinstrument 16 viainternal channel 52 and aconnector element 54. The aspirating catheter 50 (shown in FIG. 1) is connected to a vacuum aspirating unit (not shown). - In operation, the position detection unit monitors the position of the
medical instrument 16 with respect to thereference unit 36. Theregistration unit 24 correlates the changes in position of theinstrument 16 with the spacial orientation of the stored images. As the surgeon moves themedical instrument 16, images appear on thedisplay 20 responsive to the position of themedical instrument 16. This permits the surgeon to always have available the coronal, sagittal, and axial views associated with the precise location of thetip 48 of theinstrument 16 regardless of whether thetip 48 is inside of thepatient 14. Moreover, since the field generator is attached to the patient's head, the patient is free to be moved without loss of the tracking capabilities. Thedisplay 20 may further identify the location of thetip 48 on each of the displayed images as shown at 56 in FIG. 1. In other embodiments the orientation of the aspiratingtube 46 may also be identified on the displayed images. In further embodiments, a three dimensional composite image may be displayed based on the prerecorded images. - As shown in FIGS. 7-11 another embodiment of a removable
remote sensor unit 58 may be used with an aspiratingdevice 60. Thesensor unit 58, including twosensors device 60 by first engagingrecesses 66 on theunit 58 withfingers 68 on thedevice 60. Atounge 70 on theunit 58 is then received between hinge posts 72 on thedevice 60, and finally secured in place by rotating thelock 74 from an open position as shown in FIG. 8 to a closed position as shown in FIG. 7. Thelock 74 includes a recessed area at 76 adapted to frictionally engage thetounge 70 on thesensor unit 58. - The
sensor unit 58 further includes the ability to identify which of a plurality of medical instruments is attached to thesensor unit 58 at any time. Specifically, theunit 58 includes a plurality ofHall effect transistors 78, and themedical instrument 60 includes one or more tinypermanent magnets 80. By the number and/or positioning of themagnets 80, thetransistors 78 identify which of the medical instruments is attached to thesensor unit 58. - For example, if all of the
transistors 78 sense the presence of amagnet 80 then theinstrument 60 shown in FIGS. 7-11 is known to be attached to thesensor unit 58 since theinstrument 60 includes three magnets. If only twomagnets 82 are sensed then the medical instrument attached to thesensor unit 58 is adifferent instrument 84 as shown in FIG. 12. If no magnets are sensed then it is known that thesensor unit 58 is not attached to any medical instrument. Knowing the identity of the attached medical instrument permits the system to automatically adjust the position detection unit to compensate for the differences in instrument tip position with respect to the position of thesensors - As illustrated in FIGS. 13 and 14 the registration process involves two fundamental steps: 1) recording the scan images of a predetermined orientation and 2) mapping the special orientation of the position detection system onto the recorded images. For example, the orientations of the prerecorded images may be in the sagittal (i-j plane), coronal (k-j plane) and/or axial (k-i plane) as shown in FIG. 13. The images may be digitally stored and the distance between each scanned image is recorded, as are the relative orientations of each set of images. As those skilled in the art will appreciate, in alternative embodiments certain of the images may be created from other images without the need to prerecord each of the sagittal, coronal and axial views. For example, by multiplanar reformatting the sagittal and coronal images may be created from the axial images.
- In one embodiment,
fiducial markers 90 are placed on the patient'shead 14 prior to scanning with thescanner 92. The markers then appear on certain of the scanned images, and may be located by the position detection system as shown in FIG. 14. Specifically, when eachmarker 90 is sequentially located, for example with thetip 48 of amedical instrument 16, the user locates the same marker on the prerecorded images by using, for example a computer mouse. The user then controls the entering of the registration data through either acomputer keyboard 94, a mouse, or a foot switch. In alternative embodiments the registration unit may scan each prerecorded digital image beginning from one corner until it locates the identified marker. - In further embodiments involving the use of fiducial markers that are placed on the patient's body (e.g., face) prior to recording the scan images,
fiducial markers 90′ may be adhered to intermediate adhesive strips 91 which are directly adhered to the patient'sskin 93 as shown in FIGS. 15 and 16. - The
fiducial markers 90′ include aradiopaque element 95 and thestrips 91 include a small puncture hole orother marker 97. With reference to FIG. 17, the process of using thefiducial markers 90′ begins (step 1700) by first placing thestrips 91 on the patient's skin (step 1710). Thefiducial markers 90′ are then placed on thestrips 91 such that theradiopaque elements 95 align with themarkers 97 on the strips 91 (step 1704). The scan images are then recorded (step 1706), and thefiducial markers 90′ may then be removed from the patient (step 1708). During manual registration the surgeon or technician may locate themarkers 97 with the tip of a pointer (step 1710) and thereby record the positions of the fiducial markerradiopaque elements 95 with respect to the transmitter. The use of theintermediate strips 91 not only provides increased comfort to the patient after the image scanning and prior to surgery, but also facilitates accurate registration. Since theradiopaque elements 95 were centered directly on top of themarkers 93, the accuracy of registration is enhanced because the user may now locate the smallersized markers 93 instead of more indefinitely locating a portion of the larger sizedradiopaque elements 95 with the pointer tip. - Once each of the markers has been located using the position detection unit, the registration unit generates, a mapping function to translate the position detection data (in x-y-z coordinates) to the stored image orientation data (in i-j-k coordinates). In particular, the mapping equation is determined by using Powell's method as follows.
-
-
-
-
- such that (i c-ii)2+(jc-ji)2+(kc-ki)2 is a minimum for the summation of all of the collected image points. The optimization method employs distance minimization, and at least three image points are required for this method.
- The optimal values for the transformation matrices comprise the transformation equation and may now be used to translate the position of the medical instrument with respect to the transmitter in the x-y-z coordinate system, to the appropriate orientation of the prerecorded images in the i-j-k coordinate system.
- A further embodiment of the headset of the invention may be employed in an automatic registration process. For example, as shown in FIGS. 18 and 19 another embodiment of a
headset 100 of the invention includes two ear mounts 28,side members 30, and anose bridge mount 32 oncenter member 34 as discussed above with reference to FIGS. 2-4. Theheadset 100 further includes acenter plate 102 on thecenter member 34. Thecenter plate 102 is adapted to receive atransmitter 104 as shown in phantom in FIG. 19 and shown from the underside of theplate 102 in FIG. 21. Thetransmitter 104 includes twoposts 106 and a key 108 that is free to rotate about apin 110. - To install the
transmitter 104 on thecenter plate 102, the key is passed through alongitudinal opening 112 in theplate 102, and theposts 106 are each received bypost openings 114. One of thepost openings 114 is preferably formed as a slot to provide a snug fit for the transmitter yet still accommodate variations between headsets due to manufacturing tolerances. The key 108 may then be rotated to lock the transmitter onto the outer facing surface of theplate 102. Thetransmitter 104 may then be removed from and reattached to identical headsets in the same location and orientation with a high degree of accuracy. - The
headset 100 further includes very small (e.g., about 2 mm dia.) metalfiducial balls 116 secured within thecenter plate 102 as shown in FIG. 18. The automatic registration process locates theballs 116 on the prerecorded scan images, and knowing the spacial relationship between theballs 116 and thetransmitter 104, automatically generates the mapping function to translate from the transmitter coordinate system to the image coordinate system. - Specifically and with reference to FIG. 22, the automatic registration process begins (step 2200) by loading the prerecorded images (step 2202) and then creating a three dimensional data set (step 2204). Pixels having an intensity within a certain range are then identified (step 2206), and groups of adjacent pixels are located (step 2208) and classified together as a single group. The volume of each group is calculated (step 2210) and groups not within a predefined range of volumes are rejected (step 2212). Groups not having at least one pixel with an intensity level of at least a certain amount are rejected (step 2214). If the number of groups remaining is less than the number of fiducial balls 116 (step 2216), e.g., 7, then the program ends having failed to provide automatic registration (
steps 2218 and 2220). - The center of each group is then located and the distances between each group's center and the other centers are calculated and recorded in a matrix of at least 7 by 7 (step 2222). The known distances between the fiducial balls comprise a predefined 7 by 7 matrix. The program then compares each of the known distances with the various predefined distances between the fiducial balls, then generates a best fit approximation of the correlation between the sets of distances (step 2224). If the distance correlation provides an approximation outside of a preset tolerance (step 2226) then the program ends (
steps 2218 and 2220) having failed to automatically generate the transformation matrices. If the correlation of distances is within tolerance and there are seven groups (step 2228) then the image data is, recorded in the image matrix (step 2230). If the number of groups is above seven, then a geometry correlation is performed comparing the geometry of the groups to the known geometry of the fiducial balls (step 2232). If the geometry correlation is successful (step 2234) then the transformation matrices are recorded (step 2230), and if not the program reports the error condition (step 2218). - Having successfully generated the image point matrix (step 2230), and since the sensor point matrix is based on the known layout of the fiducial markers with respect to the transmitter, the mapping equation may now be automatically generated as discussed above with reference to Powell's method.
- In other embodiments wherein the patient is wearing a reference unit when the scan images are prerecorded the registration program may automatically locate portions of the reference unit itself on the scanned images, thereby identifying the orientation of the reference unit with respect to the scanned images. Again, since the relative orientation of the field generator with respect to the reference unit is known, the registration unit may then generate the appropriate mapping function. In further embodiments the surfaces of the patient's skin may be tracked such as by a laser light pointer or a movable tip pointer that is biased in a forward direction. The tracked surfaces may then be located on the stored images. In still further embodiments, the registration unit could be programmed to identify characteristic structures or features of the patient's body and thereby provide fully automatic registration. For example, the system might, knowing the size and shape of a headset, identify where the headset would be placed on the patient's head, even though it does not appear on the prerecorded images.
- The position detection system may operate by any desired principle suitable for generating a field in which position detection may be achieved at any location within the field. For example, it has been found that the 3 Spaces Fastrak™ product sold by Polhemus, Incorporated of Colchester, Vermont operates via principles suitable for use in the present invention. This product uses three orthogonally disposed magnetic dipoles for both the transmitter and the sensor, and produces alternating electromagnetic fields of 8-14 kHz that are time division multiplexed.
- Specifically and with reference to FIG. 23, both the
magnetic field source 101 and themagnetic field sensor 103 include three orthogonally disposed coils as shown. An alternating electric current from anamplifier 105 is passed through each of the source coils one at a time generating sequential magnetic fields. Aprocessing unit 107 generates the timing signals and controls a digital-to-analog converter 109. The magnetic fields induce voltages in the three coils of thesensor 103. The induced voltages are amplified by anamplifier 111, digitized by an analog-to-digital converter 113, and then processed by theprocessing unit 107. - The time division multiplexed excitation of the three coils of the source creates a unique magnetic field sequence throughout the field of the source. For every location in the field of the source, the six degree of freedom data can be calculated from the data present on the three coils of the sensor. The six degree of freedom information is then sent to a
host computer 115. - The position of a sensor S with respect to the field generator defining a reference coordinate frame (X,Y,Z) may be produced by the 3 Space® Fastrak™ product at a given time as a set of six values x s, ys, zs, ωazs, ωels, and ωros. The values xs, ys, and zs identify the position of the center of the sensor within the X,Y,Z coordinate reference frame, and the angles ωazs, ωels, and ωros identify the orientation of the-sensor S with respect to the X,Y,Z coordinate reference frame.
- The value ω azs is the azimuth angle of the sensor. The azimuth angle identifies the amount of rotation of the X and Y reference axes together about the Z axis to a new position in which the X axis is aligned with the center of the sensor in the Z direction. The new positions of the X and Y axes are defined as X′ and Y′ respectively. The value ωels is the elevation angle of the sensor. The elevation angle identifies the amount of rotation of the X′ and Z axes together about the Y′ axis to a new position in which the X′ axis is aligned with the center of the sensor S. The new positions of the X′ and Z axes are defined as X″ and Z′ respectively.
- The value ω ros is the roll angle of the sensor. The roll angle identifies the amount of rotation of the Y′ and Z′ axes together about the X″ axis to a new position defining new axes Y″ and Z″ respectively. The sensor is oriented in the X″,Y″,Z″ reference frame, and this orientation is defined by the values ωazs, ωels, and ωros.
- The combined power of all the sensor data is inversely proportional to the distance of the sensor from the source. The ratio between the sensor data components, created by the individual source coils, will determine the x, y, z position coordinate of the sensor. The ratio between the individual sensor coil data will determine the orientation of the sensor.
- Because the medical instrument is free to move with respect to the transmitter at speeds that may be faster than the rate at which the electronics can process the information, the speed of the instrument should be monitored. If the speed of movement of the instrument is above a defined threshold, then inconsistent sensor readings should be ignored until the speed falls below the threshold. The speed may be monitored by calculating a weighted sum of the differences between each of the x, y, and z coordinates at successive time intervals t 1 and t2.
- The presence of a signal from another source, or the magnetic field of the eddy current in a conductive object, or the field distorting effect of a ferro-magnetic object will change the magnitude/direction of the original magnetic field of the source. This will result in an error in the sensor position/orientation.
- In a preferred embodiment involving field integrity detection and with reference to FIGS. 1-3, a
reference sensor 37 may be securely mounted on thetransmitter assembly 12 at a fixed distance from the center of thetransmitter 36. The location and orientation of this reference sensor should be determined through a calibration process under controlled conditions, and thereafter continuously calculated and verified. In certain embodiments a weighted sum of all six sensor output parameters xs, ys, Zs, ωazs, ωels, and ωros may be continuously monitored as an indication of compromised field integrity. - As also noted above and shown in FIGS. 7-12, the
remote sensor 58 may include a plurality of sensors (62,64) the outputs of which are compared for error detection purposes. Potential error conditions that would be detectable by such a system include sensor failure where one sensor ceases to operate properly, as well as uneven localized field distortions in the area of the medical instrument. - It has further been found that simply comparing the sensor outputs may not sufficiently identify all types of error conditions that can occur, even if the distance between the sensors is taken into account. Such a potentially undetectable error condition may exist when a foreign ferromagnetic object enters the electromagnetic field and produces identical distortions at each of the sensors. This may be the case, for example if the foreign object has uniform ferromagnetic properties, if the foreign object approaches the two sensors from the same distance and at the same rate, and if the sensors are equidistant from the generator.
- In this situation the outputs of the sensors would produce identical outputs and an error detection signal might therefore not be produced even though a foreign object would be in the electromagnetic field altering the electromagnetic field as well as the sensed position data. Although the use of additional sensors may reduce the risk of this occurring, it does not eliminate the possibility of an error condition being undetected.
- It has been discovered that an error detection system sufficient to identify localized uniform distortions in the area of the medical instrument or headset may be designed using two sensors separated by a fixed distance as shown in FIGS. 7-12 and by monitoring the locations of two or more virtual points. As shown in FIG. 25, the sensors S1 and S2 are separated from each other by a
distance 2d and for convenience defined to be positioned along an axis such as the Y axis as shown. Sensor S1 uniquely defines an X-Z plane in which it is located, and S2 uniquely defines an X-Z plane in which it is located as shown. A first virtual location va is chosen to be between the X-Z planes defined by the sensors, while a second virtual location vb is chosen to be outside of the X-Z planes defined by the sensors as shown in FIG. 11. The locations va and vb are virtual locations that are continuously calculated and compared with factory defined positions. - In the embodiment diagrammatically shown in FIGS. 24 and 25 the virtual points v a (-d,-d,-d with respect to S2) and vb (d,d,d with respect to S2) are equidistant from S2. The sensor S2 is the protected sensor in this embodiment, and the sensor S1 is used as a reference to provide the error detection for S2 The magnitude of the resultant vector from S2 to va is the same as that from S2 to Vb but opposite in direction, and this magnitude is approximately one half of the distance between S1 and S2.
- The locations of v a and Vb in the reference coordinate system (i.e., with respect to S1) must be calculated and will be referred to as va1 and Vb1 The location (PS) and the orientation of the protected sensor (S1) with respect to the reference sensor must be determined. The attitude matrix (A) is calculated from the orientation values of the protected sensor:
- Then the locations of the virtual points are calculated as:
- v a1 =A·v a2 +PS
- v b1 =A·v b2 +PS
- To establish a reference value for the virtual point location in the reference sensor coordinate system, a measurement is taken in a distortion free environment during factory calibration. These stored reference values are called v ae and Vbe . Throughout the use of the system, the actual measured values of the virtual points (vam, vbm) are compared to the stored reference values for the virtual points (vae, vbe). If the distance between the established and measured location (Δ) for either virtual point is larger than a preset value (ε), then a field integrity violation message is displayed and normal operation of the system is suspended. In particular and with reference to FIG. 26
- |v alm −v alm|>εor |vblm−vble>ε
- The operation is based in part on the principle that if the position error is being reduced by the orientation error at one virtual point, then the error will be increased at the other virtual point causing a field integrity violation signal to be generated. If for example, there is an error in the measured position and orientation of the protected sensor, then the measured value will have an error added to the established value. The field integrity checking is performed in this case as follows:
- |((A e +A mΔ)·v a2 +PS e +PS mΔ)−(A e ·v a2 +PS e)|>ε
- or
- |((A e +A mΔ)·v b2 +PS e +PS mΔ)−(A e ·v b2 +PS e)|>ε
- which equals
- |A mΔ ·v a2 +PS mΔ|>ε
- or
- |A mΔ ·v b2 +PS mΔ|>ε
- Substituting
- A mΔ ·v a2 =OPS amΔand A mΔ v b2 =OPS bmΔ
- this relationship may be diagrammatically illustrated as shown in FIG. 27. The tip location of the medical instrument should be initially defined with respect to the protected sensor (S2), and used in determining the position of the tip with respect to the source.
- The integrity of the field generated by the field generator may be monitored as discussed above by positioning a reference sensor a fixed distance from the generator, and continuously monitoring its position for any changes. The calculations involved in the above field integrity detection analysis regarding the two sensors S 1 and S2 may be performed for a transmitter and single sensor field integrity detection system. Specifically, the calculations may be performed by substituting the field transmitter for the protected sensor (S2), and by substituting the single sensor for the reference sensor (S1). These field integrity analyses may also be used to identify the half field of the operation environment.
- As shown in FIG. 28 in alternative embodiments of the invention a
reference unit 120, including afield generator 122, may be positioned a small distance away from the portion of the patient's body (such as the head) 14 on an articulatedarm 124. Aheadset 12 including areference sensor 126 may be attached to the patient's body, and themedical instrument 16 may include aremote sensor 40 as discussed above with reference to FIGS. 1-6. Once thefield generator 122 is positioned at a convenient location it may be fixed in place by securing the joints of the articulated arm. The position of the patient with respect to the field generator may accordingly be monitored. The position of theinstrument 16 with respect to the patient may also be determined and the system may then operate to display the appropriate prerecorded images as discussed below. - In various embodiments, the position of the field generator 88 may be adjusted during the surgical operation by moving the articulated joints. If neither the
remote sensor 40 nor thereference sensor 126 are moved with respect to one another, then moving thefield generator 122 should not affect the position detection system. If the accuracy of the system depends at all on the relative positions of thefield generators 122 and thesensors field generator 122 during the surgical operation. This may be the case, for example, if the system relies on the near-field characteristics of a multiplexed magnetic field wherein it might be desirable to keep thesensors generator 122. In still further embodiments, the system may periodically prompt the user to reposition thegenerator 122 such as through visual cues on the display. Those skilled in the art will appreciate that the relative positioning of the field generator and the one or more field sensors is in no way limited to those shown. - The monitoring of the position of the patient may be accomplished by means other than using a headset and reference sensor. For example, a
camera 128 connected to animage processor 130 may be positioned to record the location of the field generator with respect to the target operation site of the patient as shown in FIG. 29. If either the patient or the field generator is moved, theimage processor 130 will identify the amount of relative change in location and advise theposition detection unit 22 accordingly. Additional cameras positioned to view the patient from a variety of directions may be employed in further embodiments. - As shown in FIG. 30 in an alternate embodiment, the system may include a
flexible band 132 for secure attachment to a portion of a patient's body 14 (e.g., a head or chest). Theband 132 includesfield generator 134 and areference sensor 136 that provides feedback to the signal generator in theposition detection unit 22. Theposition detection unit 22 is connected viacommunication lines 138 to theflexible band 132, and is connected viacommunication lines 140 to a flexiblemedical instrument 142 having a remote sensor at itstip 144. Because themedical instrument 142 is not rigid, the sensor should be positioned sufficiently close to the tip of theinstrument 142 to provide accurate position detection and monitoring within the patient's body. Thedisplay 20 may indicate the relative orientation of theinstrument 142 on one or more images as shown. - As shown in FIGS. 31 and 32 a system of the invention may include a flexible
medical instrument 150 having asensor 152 at itsdistal tip 154, and afiber optic endoscope 156 having asensor 158 at it distal tip. 160. Thefiber optic endoscope 156 is connected at its proximal end to acamera 162 which is in communication with animage processor 164. Because thefield generator 134 on thereference band 132 may move, for example as the patient breaths, the location of theremote sensor 152 may appear to move when in fact themedical instrument 150 has not moved. - To correct for this problem, the
fiber optic endoscope 156 can be used to monitor the position of thetip 154 of theinstrument 150 with respect to the inside of the patient's body as shown. Any sensed movement of thesensor 152 with respect to thefield generator 134 can be evaluated with reference to whether thetip 154 has moved with respect to the interior of the patient's body. If the camera observes that thetip 154 has not moved, but thesensor 152 indicates that it has moved, then the system can identify that such movement was due to the movement of the field generator and not thesensor 152. The system may then automatically correct for such variation. Further, thefiber optic endoscope 156 itself may include asensor 158 for detecting whether thetip 160 of the fiber optic has moved. This should further enhance the accuracy of the correction system. Also, thecamera 162 may provide continuous registration of the prerecorded images based on the internal structure of the patient's body. - It will be understood by those skilled in the art that numerous variations and modifications may be made to the above described embodiments without departing from the spirit and scope of the present invention.
Claims (29)
Priority Applications (3)
| Application Number | Priority Date | Filing Date | Title |
|---|---|---|---|
| US10/427,472 US20040024309A1 (en) | 1994-09-15 | 2003-04-30 | System for monitoring the position of a medical instrument with respect to a patient's body |
| US11/207,306 US20060036151A1 (en) | 1994-09-15 | 2005-08-19 | System for monitoring a position of a medical instrument |
| US11/602,640 US8473026B2 (en) | 1994-09-15 | 2006-11-21 | System for monitoring a position of a medical instrument with respect to a patient's body |
Applications Claiming Priority (6)
| Application Number | Priority Date | Filing Date | Title |
|---|---|---|---|
| US08/306,818 US5829444A (en) | 1994-09-15 | 1994-09-15 | Position tracking and imaging system for use in medical applications |
| US08/527,517 US5803089A (en) | 1994-09-15 | 1995-09-13 | Position tracking and imaging system for use in medical applications |
| US08/637,289 US5873822A (en) | 1994-09-15 | 1996-04-24 | Automatic registration system for use with position tracking and imaging system for use in medical applications |
| US09/212,024 US6175756B1 (en) | 1994-09-15 | 1998-12-15 | Position tracking and imaging system for use in medical applications |
| US09/643,608 US6694167B1 (en) | 1994-09-15 | 2000-08-22 | System for monitoring a position of a medical instrument with respect to a patient's head |
| US10/427,472 US20040024309A1 (en) | 1994-09-15 | 2003-04-30 | System for monitoring the position of a medical instrument with respect to a patient's body |
Related Parent Applications (1)
| Application Number | Title | Priority Date | Filing Date |
|---|---|---|---|
| US09/643,608 Continuation US6694167B1 (en) | 1994-09-15 | 2000-08-22 | System for monitoring a position of a medical instrument with respect to a patient's head |
Related Child Applications (1)
| Application Number | Title | Priority Date | Filing Date |
|---|---|---|---|
| US11/207,306 Continuation US20060036151A1 (en) | 1994-09-15 | 2005-08-19 | System for monitoring a position of a medical instrument |
Publications (1)
| Publication Number | Publication Date |
|---|---|
| US20040024309A1 true US20040024309A1 (en) | 2004-02-05 |
Family
ID=56289653
Family Applications (12)
| Application Number | Title | Priority Date | Filing Date |
|---|---|---|---|
| US08/527,517 Expired - Lifetime US5803089A (en) | 1994-09-15 | 1995-09-13 | Position tracking and imaging system for use in medical applications |
| US08/638,945 Expired - Lifetime US5676673A (en) | 1994-09-15 | 1996-04-24 | Position tracking and imaging system with error detection for use in medical applications |
| US08/637,131 Expired - Lifetime US5800352A (en) | 1994-09-15 | 1996-04-24 | Registration system for use with position tracking and imaging system for use in medical applications |
| US08/637,289 Expired - Lifetime US5873822A (en) | 1994-09-15 | 1996-04-24 | Automatic registration system for use with position tracking and imaging system for use in medical applications |
| US09/212,024 Expired - Lifetime US6175756B1 (en) | 1994-09-15 | 1998-12-15 | Position tracking and imaging system for use in medical applications |
| US09/643,608 Expired - Lifetime US6694167B1 (en) | 1994-09-15 | 2000-08-22 | System for monitoring a position of a medical instrument with respect to a patient's head |
| US09/643,815 Expired - Fee Related US6738656B1 (en) | 1994-09-15 | 2000-08-22 | Automatic registration system for use with position tracking an imaging system for use in medical applications |
| US09/643,271 Expired - Lifetime US6687531B1 (en) | 1994-09-15 | 2000-08-22 | Position tracking and imaging system for use in medical applications |
| US09/686,188 Expired - Fee Related US6341231B1 (en) | 1994-09-15 | 2000-10-11 | Position tracking and imaging system for use in medical applications |
| US10/427,472 Abandoned US20040024309A1 (en) | 1994-09-15 | 2003-04-30 | System for monitoring the position of a medical instrument with respect to a patient's body |
| US11/207,306 Abandoned US20060036151A1 (en) | 1994-09-15 | 2005-08-19 | System for monitoring a position of a medical instrument |
| US11/602,640 Expired - Fee Related US8473026B2 (en) | 1994-09-15 | 2006-11-21 | System for monitoring a position of a medical instrument with respect to a patient's body |
Family Applications Before (9)
| Application Number | Title | Priority Date | Filing Date |
|---|---|---|---|
| US08/527,517 Expired - Lifetime US5803089A (en) | 1994-09-15 | 1995-09-13 | Position tracking and imaging system for use in medical applications |
| US08/638,945 Expired - Lifetime US5676673A (en) | 1994-09-15 | 1996-04-24 | Position tracking and imaging system with error detection for use in medical applications |
| US08/637,131 Expired - Lifetime US5800352A (en) | 1994-09-15 | 1996-04-24 | Registration system for use with position tracking and imaging system for use in medical applications |
| US08/637,289 Expired - Lifetime US5873822A (en) | 1994-09-15 | 1996-04-24 | Automatic registration system for use with position tracking and imaging system for use in medical applications |
| US09/212,024 Expired - Lifetime US6175756B1 (en) | 1994-09-15 | 1998-12-15 | Position tracking and imaging system for use in medical applications |
| US09/643,608 Expired - Lifetime US6694167B1 (en) | 1994-09-15 | 2000-08-22 | System for monitoring a position of a medical instrument with respect to a patient's head |
| US09/643,815 Expired - Fee Related US6738656B1 (en) | 1994-09-15 | 2000-08-22 | Automatic registration system for use with position tracking an imaging system for use in medical applications |
| US09/643,271 Expired - Lifetime US6687531B1 (en) | 1994-09-15 | 2000-08-22 | Position tracking and imaging system for use in medical applications |
| US09/686,188 Expired - Fee Related US6341231B1 (en) | 1994-09-15 | 2000-10-11 | Position tracking and imaging system for use in medical applications |
Family Applications After (2)
| Application Number | Title | Priority Date | Filing Date |
|---|---|---|---|
| US11/207,306 Abandoned US20060036151A1 (en) | 1994-09-15 | 2005-08-19 | System for monitoring a position of a medical instrument |
| US11/602,640 Expired - Fee Related US8473026B2 (en) | 1994-09-15 | 2006-11-21 | System for monitoring a position of a medical instrument with respect to a patient's body |
Country Status (5)
| Country | Link |
|---|---|
| US (12) | US5803089A (en) |
| EP (1) | EP0951874A3 (en) |
| JP (1) | JP3325533B2 (en) |
| AT (1) | ATE252349T1 (en) |
| DE (1) | DE69531994T2 (en) |
Cited By (105)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| US20020156363A1 (en) * | 1999-10-28 | 2002-10-24 | Hunter Mark W. | Registration of human anatomy integrated for electromagnetic localization |
| US20020188172A1 (en) * | 1997-04-16 | 2002-12-12 | Klaus Irion | Endoscopic system |
| US20030073901A1 (en) * | 1999-03-23 | 2003-04-17 | Simon David A. | Navigational guidance via computer-assisted fluoroscopic imaging |
| US20030114752A1 (en) * | 1999-04-20 | 2003-06-19 | Jaimie Henderson | Instrument guidance method and system for image guided surgery |
| US20030117135A1 (en) * | 1999-10-28 | 2003-06-26 | Martinelli Michael A. | Method and system for navigating a catheter probe in the presence of field-influencing objects |
| US20040087852A1 (en) * | 2001-02-06 | 2004-05-06 | Edward Chen | Computer-assisted surgical positioning method and system |
| US20040097806A1 (en) * | 2002-11-19 | 2004-05-20 | Mark Hunter | Navigation system for cardiac therapies |
| US20040097805A1 (en) * | 2002-11-19 | 2004-05-20 | Laurent Verard | Navigation system for cardiac therapies |
| US20040152972A1 (en) * | 2003-01-30 | 2004-08-05 | Mark Hunter | Method and apparatus for post-operative tuning of a spinal implant |
| US20040171924A1 (en) * | 2003-01-30 | 2004-09-02 | Mire David A. | Method and apparatus for preplanning a surgical procedure |
| US20040181149A1 (en) * | 2001-02-07 | 2004-09-16 | Ulrich Langlotz | Device and method for intraoperative navigation |
| US20040215071A1 (en) * | 2003-04-25 | 2004-10-28 | Frank Kevin J. | Method and apparatus for performing 2D to 3D registration |
| US20050059885A1 (en) * | 1997-12-12 | 2005-03-17 | Tony Melkent | Image guided spinal surgery guide, system and method for use thereof |
| US20050085714A1 (en) * | 2003-10-16 | 2005-04-21 | Foley Kevin T. | Method and apparatus for surgical navigation of a multiple piece construct for implantation |
| US20050085720A1 (en) * | 2003-10-17 | 2005-04-21 | Jascob Bradley A. | Method and apparatus for surgical navigation |
| US20050113809A1 (en) * | 2000-03-01 | 2005-05-26 | Melkent Anthony J. | Multiple cannula image guided tool for image guided procedures |
| US20050165292A1 (en) * | 2002-04-04 | 2005-07-28 | Simon David A. | Method and apparatus for virtual digital subtraction angiography |
| US20050245817A1 (en) * | 2004-05-03 | 2005-11-03 | Clayton John B | Method and apparatus for implantation between two vertebral bodies |
| US20050273004A1 (en) * | 2002-02-28 | 2005-12-08 | Simon David A | Method and apparatus for perspective inversion |
| US20060025677A1 (en) * | 2003-10-17 | 2006-02-02 | Verard Laurent G | Method and apparatus for surgical navigation |
| US20060058645A1 (en) * | 2004-09-01 | 2006-03-16 | Komistek Richard D | Method and apparatus for imaging tracking |
| US20060084867A1 (en) * | 2003-10-17 | 2006-04-20 | Tremblay Brian M | Method and apparatus for surgical navigation |
| US20060094958A1 (en) * | 2004-10-28 | 2006-05-04 | Marquart Joel G | Method and apparatus for calibrating non-linear instruments |
| US20060122497A1 (en) * | 2004-11-12 | 2006-06-08 | Glossop Neil D | Device and method for ensuring the accuracy of a tracking device in a volume |
| US20060173291A1 (en) * | 2005-01-18 | 2006-08-03 | Glossop Neil D | Electromagnetically tracked K-wire device |
| US20060170417A1 (en) * | 2005-02-02 | 2006-08-03 | Rodgers Allan G | Distributed array magnetic tracking |
| US20060173269A1 (en) * | 2004-11-12 | 2006-08-03 | Glossop Neil D | Integrated skin-mounted multifunction device for use in image-guided surgery |
| US20060199159A1 (en) * | 2005-03-01 | 2006-09-07 | Neuronetics, Inc. | Head phantom for simulating the patient response to magnetic stimulation |
| US20060262961A1 (en) * | 2000-06-14 | 2006-11-23 | Troy Holsing Et Al. | System and method for image based sensor calibration |
| US20060278247A1 (en) * | 1999-10-28 | 2006-12-14 | Mark W. Hunter Et Al. | Surgical communication and power system |
| US20070032723A1 (en) * | 2005-06-21 | 2007-02-08 | Glossop Neil D | System, method and apparatus for navigated therapy and diagnosis |
| US20070055128A1 (en) * | 2005-08-24 | 2007-03-08 | Glossop Neil D | System, method and devices for navigated flexible endoscopy |
| US20070066887A1 (en) * | 2005-09-21 | 2007-03-22 | Mire David A | Method and apparatus for positioning a reference frame |
| US20070167722A1 (en) * | 1992-08-14 | 2007-07-19 | British Telecommunications Public Limited Company | Surgical navigation |
| US20070167787A1 (en) * | 2005-06-21 | 2007-07-19 | Glossop Neil D | Device and method for a trackable ultrasound |
| US20070166188A1 (en) * | 2006-01-18 | 2007-07-19 | Eric Ryterski | Method and apparatus for providing a container to a sterile environment |
| US20070249911A1 (en) * | 2006-04-21 | 2007-10-25 | Simon David A | Method and apparatus for optimizing a therapy |
| US20080058630A1 (en) * | 2006-09-01 | 2008-03-06 | Robertson Timothy L | Simultaneous blood flow and hematocrit sensor |
| US20080071215A1 (en) * | 2004-11-05 | 2008-03-20 | Traxtal Technologies Inc. | Access System |
| US20080081982A1 (en) * | 2006-09-29 | 2008-04-03 | Medtronic, Inc. | Method And Apparatus For Optimizing A Computer Assisted Surgical Procedure |
| US20080097195A1 (en) * | 2003-08-28 | 2008-04-24 | Surgical Navigation Technologies, Inc. | Method and apparatus for performing stereotactic surgery |
| US20080119712A1 (en) * | 2006-11-20 | 2008-05-22 | General Electric Company | Systems and Methods for Automated Image Registration |
| US20080262297A1 (en) * | 2004-04-26 | 2008-10-23 | Super Dimension Ltd. | System and Method for Image-Based Alignment of an Endoscope |
| US20080312529A1 (en) * | 2007-06-15 | 2008-12-18 | Louis-Philippe Amiot | Computer-assisted surgery system and method |
| WO2009008894A2 (en) * | 2006-08-22 | 2009-01-15 | Dimensions Imaging | System and method for determining absolute position using a multiple wavelength signal |
| US20090287443A1 (en) * | 2001-06-04 | 2009-11-19 | Surgical Navigation Technologies, Inc. | Method for Calibrating a Navigation System |
| US20100204575A1 (en) * | 2005-11-29 | 2010-08-12 | Martin Roche | Method and system for enhancing accuracy in ultrasonic alignment |
| US20100204955A1 (en) * | 2005-11-28 | 2010-08-12 | Martin Roche | Method and system for positional measurement using ultrasonic sensing |
| US20100210939A1 (en) * | 1999-10-28 | 2010-08-19 | Medtronic Navigation, Inc. | Method and Apparatus for Surgical Navigation |
| US7853305B2 (en) | 2000-04-07 | 2010-12-14 | Medtronic Navigation, Inc. | Trajectory storage apparatus and method for surgical navigation systems |
| US20110032184A1 (en) * | 2005-12-01 | 2011-02-10 | Martin Roche | Orthopedic method and system for mapping an anatomical pivot point |
| USRE42194E1 (en) | 1997-09-24 | 2011-03-01 | Medtronic Navigation, Inc. | Percutaneous registration apparatus and method for use in computer-assisted surgical navigation |
| US20110060220A1 (en) * | 2005-12-01 | 2011-03-10 | Martin Roche | Virtual mapping of an anatomical pivot point and alignment therewith |
| US20110160572A1 (en) * | 2009-12-31 | 2011-06-30 | Orthosensor | Disposable wand and sensor for orthopedic alignment |
| US7998062B2 (en) | 2004-03-29 | 2011-08-16 | Superdimension, Ltd. | Endoscope structures and techniques for navigating to a target in branched structure |
| US20110207997A1 (en) * | 2009-04-08 | 2011-08-25 | Superdimension, Ltd. | Locatable Catheter |
| US8057407B2 (en) | 1999-10-28 | 2011-11-15 | Medtronic Navigation, Inc. | Surgical sensor |
| US20120070046A1 (en) * | 2010-09-20 | 2012-03-22 | Siemens Corporation | Method and System for Detection and Tracking of Coronary Sinus Catheter Electrodes in Fluoroscopic Images |
| US8165658B2 (en) | 2008-09-26 | 2012-04-24 | Medtronic, Inc. | Method and apparatus for positioning a guide relative to a base |
| USRE43328E1 (en) | 1997-11-20 | 2012-04-24 | Medtronic Navigation, Inc | Image guided awl/tap/screwdriver |
| US8175681B2 (en) | 2008-12-16 | 2012-05-08 | Medtronic Navigation Inc. | Combination of electromagnetic and electropotential localization |
| US20120136626A1 (en) * | 2009-05-18 | 2012-05-31 | Dirk Mucha | Method for generating position data of an instrument |
| USRE43952E1 (en) | 1989-10-05 | 2013-01-29 | Medtronic Navigation, Inc. | Interactive system for local intervention inside a non-homogeneous structure |
| US20130072788A1 (en) * | 2011-09-19 | 2013-03-21 | Siemens Aktiengesellschaft | Method and System for Tracking Catheters in 2D X-Ray Fluoroscopy Using a Graphics Processing Unit |
| US8421642B1 (en) | 2006-08-24 | 2013-04-16 | Navisense | System and method for sensorized user interface |
| US8452068B2 (en) | 2008-06-06 | 2013-05-28 | Covidien Lp | Hybrid registration method |
| US8473032B2 (en) | 2008-06-03 | 2013-06-25 | Superdimension, Ltd. | Feature-based registration method |
| US8494613B2 (en) | 2009-08-31 | 2013-07-23 | Medtronic, Inc. | Combination localization system |
| US8494805B2 (en) | 2005-11-28 | 2013-07-23 | Orthosensor | Method and system for assessing orthopedic alignment using tracking sensors |
| US8494614B2 (en) | 2009-08-31 | 2013-07-23 | Regents Of The University Of Minnesota | Combination localization system |
| US8547248B2 (en) | 2005-09-01 | 2013-10-01 | Proteus Digital Health, Inc. | Implantable zero-wire communications system |
| US8603014B2 (en) | 2010-10-05 | 2013-12-10 | Cerevast Therapeutics, Inc. | Hands-free operator-independent transcranial ultrasound apparatus and methods |
| US8611983B2 (en) | 2005-01-18 | 2013-12-17 | Philips Electronics Ltd | Method and apparatus for guiding an instrument to a target in the lung |
| US8613714B2 (en) | 2010-10-05 | 2013-12-24 | Cerevast Therapeutics, Inc. | Non-invasive transcranial ultrasound apparatus |
| US8638296B1 (en) | 2006-09-05 | 2014-01-28 | Jason McIntosh | Method and machine for navigation system calibration |
| US8663088B2 (en) | 2003-09-15 | 2014-03-04 | Covidien Lp | System of accessories for use with bronchoscopes |
| US8764725B2 (en) | 2004-02-09 | 2014-07-01 | Covidien Lp | Directional anchoring mechanism, method and applications thereof |
| US8768437B2 (en) | 1998-08-20 | 2014-07-01 | Sofamor Danek Holdings, Inc. | Fluoroscopic image guided surgery system with intraoperative registration |
| US8905920B2 (en) | 2007-09-27 | 2014-12-09 | Covidien Lp | Bronchoscope adapter and method |
| US8932207B2 (en) | 2008-07-10 | 2015-01-13 | Covidien Lp | Integrated multi-functional endoscopic tool |
| US9008757B2 (en) | 2012-09-26 | 2015-04-14 | Stryker Corporation | Navigation system including optical and non-optical sensors |
| US9189083B2 (en) | 2008-03-18 | 2015-11-17 | Orthosensor Inc. | Method and system for media presentation during operative workflow |
| US9575140B2 (en) | 2008-04-03 | 2017-02-21 | Covidien Lp | Magnetic interference detection system and method |
| US10418705B2 (en) | 2016-10-28 | 2019-09-17 | Covidien Lp | Electromagnetic navigation antenna assembly and electromagnetic navigation system including the same |
| US10426555B2 (en) | 2015-06-03 | 2019-10-01 | Covidien Lp | Medical instrument with sensor for use in a system and method for electromagnetic navigation |
| US10446931B2 (en) | 2016-10-28 | 2019-10-15 | Covidien Lp | Electromagnetic navigation antenna assembly and electromagnetic navigation system including the same |
| US10478254B2 (en) | 2016-05-16 | 2019-11-19 | Covidien Lp | System and method to access lung tissue |
| US10517505B2 (en) | 2016-10-28 | 2019-12-31 | Covidien Lp | Systems, methods, and computer-readable media for optimizing an electromagnetic navigation system |
| US10582879B2 (en) | 2004-02-17 | 2020-03-10 | Philips Electronics Ltd | Method and apparatus for registration, verification and referencing of internal organs |
| US10582834B2 (en) | 2010-06-15 | 2020-03-10 | Covidien Lp | Locatable expandable working channel and method |
| US10615500B2 (en) | 2016-10-28 | 2020-04-07 | Covidien Lp | System and method for designing electromagnetic navigation antenna assemblies |
| US10638952B2 (en) | 2016-10-28 | 2020-05-05 | Covidien Lp | Methods, systems, and computer-readable media for calibrating an electromagnetic navigation system |
| US10722311B2 (en) | 2016-10-28 | 2020-07-28 | Covidien Lp | System and method for identifying a location and/or an orientation of an electromagnetic sensor based on a map |
| US10751126B2 (en) | 2016-10-28 | 2020-08-25 | Covidien Lp | System and method for generating a map for electromagnetic navigation |
| US10792106B2 (en) | 2016-10-28 | 2020-10-06 | Covidien Lp | System for calibrating an electromagnetic navigation system |
| US10952593B2 (en) | 2014-06-10 | 2021-03-23 | Covidien Lp | Bronchoscope adapter |
| WO2021074326A1 (en) * | 2019-10-15 | 2021-04-22 | Fiagon Ag Medical Technologies | Automatic medical instrument identification |
| US11006914B2 (en) | 2015-10-28 | 2021-05-18 | Medtronic Navigation, Inc. | Apparatus and method for maintaining image quality while minimizing x-ray dosage of a patient |
| US11164679B2 (en) | 2017-06-20 | 2021-11-02 | Advinow, Inc. | Systems and methods for intelligent patient interface exam station |
| US11219489B2 (en) | 2017-10-31 | 2022-01-11 | Covidien Lp | Devices and systems for providing sensors in parallel with medical tools |
| US11331150B2 (en) | 1999-10-28 | 2022-05-17 | Medtronic Navigation, Inc. | Method and apparatus for surgical navigation |
| US11348688B2 (en) * | 2018-03-06 | 2022-05-31 | Advinow, Inc. | Systems and methods for audio medical instrument patient measurements |
| US11357574B2 (en) | 2013-10-31 | 2022-06-14 | Intersect ENT International GmbH | Surgical instrument and method for detecting the position of a surgical instrument |
| US11430139B2 (en) | 2019-04-03 | 2022-08-30 | Intersect ENT International GmbH | Registration method and setup |
| US20220287635A1 (en) * | 2021-03-10 | 2022-09-15 | Livivos Inc. | Systems and methods for non-invasive fat composition measurement in an organ |
Families Citing this family (731)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| US6347240B1 (en) | 1990-10-19 | 2002-02-12 | St. Louis University | System and method for use in displaying images of a body part |
| US5603318A (en) | 1992-04-21 | 1997-02-18 | University Of Utah Research Foundation | Apparatus and method for photogrammetric surgical localization |
| US5762458A (en) | 1996-02-20 | 1998-06-09 | Computer Motion, Inc. | Method and apparatus for performing minimally invasive cardiac procedures |
| US7077822B1 (en) * | 1994-02-09 | 2006-07-18 | The University Of Iowa Research Foundation | Stereotactic hypothalamic obesity probe |
| US5829444A (en) | 1994-09-15 | 1998-11-03 | Visualization Technology, Inc. | Position tracking and imaging system for use in medical applications |
| US5803089A (en) * | 1994-09-15 | 1998-09-08 | Visualization Technology, Inc. | Position tracking and imaging system for use in medical applications |
| US6646541B1 (en) | 1996-06-24 | 2003-11-11 | Computer Motion, Inc. | General purpose distributed operating room control system |
| US6463361B1 (en) | 1994-09-22 | 2002-10-08 | Computer Motion, Inc. | Speech interface for an automated endoscopic system |
| US5695501A (en) | 1994-09-30 | 1997-12-09 | Ohio Medical Instrument Company, Inc. | Apparatus for neurosurgical stereotactic procedures |
| DE69532829T2 (en) * | 1994-10-07 | 2005-01-27 | St. Louis University | DEVICE FOR USE WITH A SURGICAL NAVIGATION SYSTEM |
| US6978166B2 (en) | 1994-10-07 | 2005-12-20 | Saint Louis University | System for use in displaying images of a body part |
| US6091058A (en) | 1995-04-26 | 2000-07-18 | O.R. Solutions, Inc. | Thermal treatment system and method for maintaining integrity and ensuring sterility of surgical drapes used with surgical equipment |
| US5592939A (en) | 1995-06-14 | 1997-01-14 | Martinelli; Michael A. | Method and system for navigating a catheter probe |
| US6702736B2 (en) * | 1995-07-24 | 2004-03-09 | David T. Chen | Anatomical visualization system |
| US5776050A (en) * | 1995-07-24 | 1998-07-07 | Medical Media Systems | Anatomical visualization system |
| US6714841B1 (en) | 1995-09-15 | 2004-03-30 | Computer Motion, Inc. | Head cursor control interface for an automated endoscope system for optimal positioning |
| US7445594B1 (en) | 1995-09-20 | 2008-11-04 | Medtronic, Inc. | Method and apparatus for temporarily immobilizing a local area of tissue |
| US6351659B1 (en) | 1995-09-28 | 2002-02-26 | Brainlab Med. Computersysteme Gmbh | Neuro-navigation system |
| US6699177B1 (en) | 1996-02-20 | 2004-03-02 | Computer Motion, Inc. | Method and apparatus for performing minimally invasive surgical procedures |
| US5971976A (en) * | 1996-02-20 | 1999-10-26 | Computer Motion, Inc. | Motion minimization and compensation system for use in surgical procedures |
| US6436107B1 (en) | 1996-02-20 | 2002-08-20 | Computer Motion, Inc. | Method and apparatus for performing minimally invasive surgical procedures |
| US5855583A (en) | 1996-02-20 | 1999-01-05 | Computer Motion, Inc. | Method and apparatus for performing minimally invasive cardiac procedures |
| US6167296A (en) * | 1996-06-28 | 2000-12-26 | The Board Of Trustees Of The Leland Stanford Junior University | Method for volumetric image navigation |
| US6009212A (en) | 1996-07-10 | 1999-12-28 | Washington University | Method and apparatus for image registration |
| US6408107B1 (en) | 1996-07-10 | 2002-06-18 | Michael I. Miller | Rapid convolution based large deformation image matching via landmark and volume imagery |
| US6611630B1 (en) | 1996-07-10 | 2003-08-26 | Washington University | Method and apparatus for automatic shape characterization |
| US6226418B1 (en) | 1997-11-07 | 2001-05-01 | Washington University | Rapid convolution based large deformation image matching via landmark and volume imagery |
| US6684098B2 (en) | 1996-08-16 | 2004-01-27 | Brigham And Women's Hospital, Inc. | Versatile stereotactic device and methods of use |
| US6605041B2 (en) * | 1996-08-22 | 2003-08-12 | Synthes (U.S.A.) | 3-D ultrasound recording device |
| US6296613B1 (en) | 1997-08-22 | 2001-10-02 | Synthes (U.S.A.) | 3D ultrasound recording device |
| US6132441A (en) | 1996-11-22 | 2000-10-17 | Computer Motion, Inc. | Rigidly-linked articulating wrist with decoupled motion transmission |
| US8206406B2 (en) | 1996-12-12 | 2012-06-26 | Intuitive Surgical Operations, Inc. | Disposable sterile surgical adaptor |
| US7666191B2 (en) | 1996-12-12 | 2010-02-23 | Intuitive Surgical, Inc. | Robotic surgical system with sterile surgical adaptor |
| US8182469B2 (en) | 1997-11-21 | 2012-05-22 | Intuitive Surgical Operations, Inc. | Surgical accessory clamp and method |
| US8529582B2 (en) | 1996-12-12 | 2013-09-10 | Intuitive Surgical Operations, Inc. | Instrument interface of a robotic surgical system |
| US7727244B2 (en) | 1997-11-21 | 2010-06-01 | Intuitive Surgical Operation, Inc. | Sterile surgical drape |
| US6331181B1 (en) * | 1998-12-08 | 2001-12-18 | Intuitive Surgical, Inc. | Surgical robotic tools, data architecture, and use |
| US6132368A (en) | 1996-12-12 | 2000-10-17 | Intuitive Surgical, Inc. | Multi-component telepresence system and method |
| US6314310B1 (en) * | 1997-02-14 | 2001-11-06 | Biosense, Inc. | X-ray guided surgical location system with extended mapping volume |
| US6006127A (en) * | 1997-02-28 | 1999-12-21 | U.S. Philips Corporation | Image-guided surgery system |
| US6702789B1 (en) | 1997-03-11 | 2004-03-09 | Alcove Medical, Inc. | Catheter having insertion control mechanism and anti-bunching mechanism |
| US6708184B2 (en) | 1997-04-11 | 2004-03-16 | Medtronic/Surgical Navigation Technologies | Method and apparatus for producing and accessing composite data using a device having a distributed communication controller interface |
| US5970499A (en) | 1997-04-11 | 1999-10-19 | Smith; Kurt R. | Method and apparatus for producing and accessing composite data |
| US6752812B1 (en) | 1997-05-15 | 2004-06-22 | Regent Of The University Of Minnesota | Remote actuation of trajectory guide |
| WO1999000052A1 (en) * | 1997-06-27 | 1999-01-07 | The Board Of Trustees Of The Leland Stanford Junior University | Method and apparatus for volumetric image navigation |
| US6212419B1 (en) * | 1997-11-12 | 2001-04-03 | Walter M. Blume | Method and apparatus using shaped field of repositionable magnet to guide implant |
| IL122336A0 (en) * | 1997-11-27 | 1998-04-05 | Ultra Guide Ltd | System and method for guiding the movements of a device to a target particularly for medical applications |
| US6860878B2 (en) | 1998-02-24 | 2005-03-01 | Endovia Medical Inc. | Interchangeable instrument |
| US8414598B2 (en) | 1998-02-24 | 2013-04-09 | Hansen Medical, Inc. | Flexible instrument |
| US7169141B2 (en) | 1998-02-24 | 2007-01-30 | Hansen Medical, Inc. | Surgical instrument |
| US6843793B2 (en) * | 1998-02-24 | 2005-01-18 | Endovia Medical, Inc. | Surgical instrument |
| US20080177285A1 (en) * | 1998-02-24 | 2008-07-24 | Hansen Medical, Inc. | Surgical instrument |
| US8303576B2 (en) * | 1998-02-24 | 2012-11-06 | Hansen Medical, Inc. | Interchangeable surgical instrument |
| US7789875B2 (en) * | 1998-02-24 | 2010-09-07 | Hansen Medical, Inc. | Surgical instruments |
| US7901399B2 (en) * | 1998-02-24 | 2011-03-08 | Hansen Medical, Inc. | Interchangeable surgical instrument |
| US7297142B2 (en) * | 1998-02-24 | 2007-11-20 | Hansen Medical, Inc. | Interchangeable surgical instrument |
| US7713190B2 (en) * | 1998-02-24 | 2010-05-11 | Hansen Medical, Inc. | Flexible instrument |
| US7758569B2 (en) | 1998-02-24 | 2010-07-20 | Hansen Medical, Inc. | Interchangeable surgical instrument |
| SE9801006D0 (en) | 1998-03-25 | 1998-03-25 | Siemens Elema Ab | Method and arrangement for determining the location of a catheter within an animal body |
| US6529765B1 (en) | 1998-04-21 | 2003-03-04 | Neutar L.L.C. | Instrumented and actuated guidance fixture for sterotactic surgery |
| US6298262B1 (en) | 1998-04-21 | 2001-10-02 | Neutar, Llc | Instrument guidance for stereotactic surgery |
| US6546277B1 (en) | 1998-04-21 | 2003-04-08 | Neutar L.L.C. | Instrument guidance system for spinal and other surgery |
| AU3754299A (en) * | 1998-04-24 | 1999-11-16 | Case Western Reserve University | Geometric distortion correction in magnetic resonance imaging |
| ATE389364T1 (en) | 1998-06-22 | 2008-04-15 | Ao Technology Ag | FIDUCIAL MATCHING USING FIDUCIAL SCREW |
| US6118845A (en) | 1998-06-29 | 2000-09-12 | Surgical Navigation Technologies, Inc. | System and methods for the reduction and elimination of image artifacts in the calibration of X-ray imagers |
| US6145509A (en) * | 1998-07-24 | 2000-11-14 | Eva Corporation | Depth sensor device for use in a surgical procedure |
| US6282437B1 (en) | 1998-08-12 | 2001-08-28 | Neutar, Llc | Body-mounted sensing system for stereotactic surgery |
| US6351662B1 (en) | 1998-08-12 | 2002-02-26 | Neutar L.L.C. | Movable arm locator for stereotactic surgery |
| US6511417B1 (en) * | 1998-09-03 | 2003-01-28 | Olympus Optical Co., Ltd. | System for detecting the shape of an endoscope using source coils and sense coils |
| US6482182B1 (en) | 1998-09-03 | 2002-11-19 | Surgical Navigation Technologies, Inc. | Anchoring system for a brain lead |
| EP1115328A4 (en) * | 1998-09-24 | 2004-11-10 | Super Dimension Ltd | System and method for determining the location of a catheter during an intra-body medical procedure |
| US6256546B1 (en) * | 1998-09-28 | 2001-07-03 | General Electric Company | System and method for numerical control processing of an in-processing part |
| WO2000021442A1 (en) | 1998-10-09 | 2000-04-20 | Surgical Navigation Technologies, Inc. | Image guided vertebral distractor |
| US6852107B2 (en) | 2002-01-16 | 2005-02-08 | Computer Motion, Inc. | Minimally invasive surgical training using robotics and tele-collaboration |
| US6659939B2 (en) | 1998-11-20 | 2003-12-09 | Intuitive Surgical, Inc. | Cooperative minimally invasive telesurgical system |
| US6951535B2 (en) | 2002-01-16 | 2005-10-04 | Intuitive Surgical, Inc. | Tele-medicine system that transmits an entire state of a subsystem |
| US6468265B1 (en) | 1998-11-20 | 2002-10-22 | Intuitive Surgical, Inc. | Performing cardiac surgery without cardioplegia |
| US6398726B1 (en) | 1998-11-20 | 2002-06-04 | Intuitive Surgical, Inc. | Stabilizer for robotic beating-heart surgery |
| DE69941305D1 (en) * | 1998-11-20 | 2009-10-01 | Intuitive Surgical Inc | System for cardiac surgery without cardioplegia |
| US8527094B2 (en) | 1998-11-20 | 2013-09-03 | Intuitive Surgical Operations, Inc. | Multi-user medical robotic system for collaboration or training in minimally invasive surgical procedures |
| EP1161691A2 (en) * | 1998-12-23 | 2001-12-12 | Peter D. Jakab | Magnetic resonance scanner with electromagnetic position and orientation tracking device |
| JP4342016B2 (en) * | 1999-01-06 | 2009-10-14 | 株式会社日立メディコ | Image display device |
| US6332891B1 (en) * | 1999-02-16 | 2001-12-25 | Stryker Corporation | System and method for performing image guided surgery |
| US7749089B1 (en) | 1999-02-26 | 2010-07-06 | Creative Kingdoms, Llc | Multi-media interactive play system |
| US6173715B1 (en) * | 1999-03-01 | 2001-01-16 | Lucent Medical Systems, Inc. | Magnetic anatomical marker and method of use |
| EP1161194B1 (en) | 1999-03-17 | 2006-04-26 | SYNTHES AG Chur | Imaging and planning device for ligament graft placement |
| DE60042321D1 (en) * | 1999-04-07 | 2009-07-16 | Univ Loma Linda Med | SYSTEM FOR MONITORING PATIENT MOVEMENTS IN PROTON THERAPY |
| AU766981B2 (en) | 1999-04-20 | 2003-10-30 | Ao Technology Ag | Device for the percutaneous obtainment of 3D-coordinates on the surface of a human or animal organ |
| EP1504726A1 (en) * | 1999-04-22 | 2005-02-09 | Medtronic Surgical Navigation Technologies | Apparatus for image guided surgery |
| AU768975B2 (en) * | 1999-05-03 | 2004-01-15 | Ao Technology Ag | Position detector with auxiliary means for detecting the direction of the gravity vector |
| US6317619B1 (en) | 1999-07-29 | 2001-11-13 | U.S. Philips Corporation | Apparatus, methods, and devices for magnetic resonance imaging controlled by the position of a moveable RF coil |
| US6773393B1 (en) * | 1999-08-05 | 2004-08-10 | Olympus Optical Co., Ltd. | Apparatus and method for detecting and displaying form of insertion part of endoscope |
| US6996430B1 (en) | 1999-08-16 | 2006-02-07 | Super Dimension Ltd | Method and system for displaying cross-sectional images of a body |
| US6368285B1 (en) * | 1999-09-21 | 2002-04-09 | Biosense, Inc. | Method and apparatus for mapping a chamber of a heart |
| US6747539B1 (en) | 1999-10-28 | 2004-06-08 | Michael A. Martinelli | Patient-shielding and coil system |
| US6235038B1 (en) | 1999-10-28 | 2001-05-22 | Medtronic Surgical Navigation Technologies | System for translation of electromagnetic and optical localization systems |
| US6379302B1 (en) | 1999-10-28 | 2002-04-30 | Surgical Navigation Technologies Inc. | Navigation information overlay onto ultrasound imagery |
| AU1240801A (en) | 1999-10-28 | 2001-05-08 | Enterprise Medical Technology, Inc. | Coil structures and methods for generating magnetic fields |
| US6400139B1 (en) * | 1999-11-01 | 2002-06-04 | Polhemus Inc. | Methods and apparatus for electromagnetic position and orientation tracking with distortion compensation |
| US6702805B1 (en) * | 1999-11-12 | 2004-03-09 | Microdexterity Systems, Inc. | Manipulator |
| DE19956814B4 (en) * | 1999-11-25 | 2004-07-15 | Brainlab Ag | Shape detection of treatment devices |
| DE60028824T2 (en) * | 1999-12-15 | 2007-01-18 | Super Dimension Ltd. | DEVICE FOR APPLYING ENERGY TO A TARGET OBJECT |
| US7747312B2 (en) * | 2000-01-04 | 2010-06-29 | George Mason Intellectual Properties, Inc. | System and method for automatic shape registration and instrument tracking |
| US20020193686A1 (en) * | 2000-01-10 | 2002-12-19 | Pinhas Gilboa | Methods and systems for performing medical procedures with reference to projective image and with respect to pre-stored images |
| US7635390B1 (en) | 2000-01-14 | 2009-12-22 | Marctec, Llc | Joint replacement component having a modular articulating surface |
| DE20002604U1 (en) * | 2000-02-15 | 2001-06-21 | Ao Entwicklungsinstitut Davos | Laser pointer |
| US7445550B2 (en) | 2000-02-22 | 2008-11-04 | Creative Kingdoms, Llc | Magical wand and interactive play experience |
| US7878905B2 (en) | 2000-02-22 | 2011-02-01 | Creative Kingdoms, Llc | Multi-layered interactive play experience |
| US6761637B2 (en) | 2000-02-22 | 2004-07-13 | Creative Kingdoms, Llc | Method of game play using RFID tracking device |
| US7366561B2 (en) * | 2000-04-07 | 2008-04-29 | Medtronic, Inc. | Robotic trajectory guide |
| US7660621B2 (en) | 2000-04-07 | 2010-02-09 | Medtronic, Inc. | Medical device introducer |
| US6585746B2 (en) | 2000-04-20 | 2003-07-01 | Philip L. Gildenberg | Hair transplantation method and apparatus |
| US6676706B1 (en) | 2000-04-26 | 2004-01-13 | Zimmer Technology, Inc. | Method and apparatus for performing a minimally invasive total hip arthroplasty |
| US6991656B2 (en) * | 2000-04-26 | 2006-01-31 | Dana Mears | Method and apparatus for performing a minimally invasive total hip arthroplasty |
| US20050043810A1 (en) * | 2000-04-26 | 2005-02-24 | Dana Mears | Method and apparatus for performing a minimally invasive total hip arthroplasty |
| US6484049B1 (en) | 2000-04-28 | 2002-11-19 | Ge Medical Systems Global Technology Company, Llc | Fluoroscopic tracking and visualization system |
| US6856826B2 (en) * | 2000-04-28 | 2005-02-15 | Ge Medical Systems Global Technology Company, Llc | Fluoroscopic tracking and visualization system |
| US6856827B2 (en) * | 2000-04-28 | 2005-02-15 | Ge Medical Systems Global Technology Company, Llc | Fluoroscopic tracking and visualization system |
| EP1153572B1 (en) * | 2000-05-09 | 2002-08-07 | BrainLAB AG | Method of registering of patient data of an imaging method for navigation supported surgical operations by means of X-ray image correspondance |
| US6860271B2 (en) * | 2000-05-17 | 2005-03-01 | O.R. Solutions, Inc. | Thermal treatment system and method for controlling the system to thermally treat sterile surgical liquid |
| US6371121B1 (en) * | 2000-05-17 | 2002-04-16 | O.R. Solutions, Inc. | Remote controlled thermal treatment system and method for controlling the system remotely to thermally treat sterile surgical liquid |
| DE10027782A1 (en) * | 2000-06-07 | 2001-12-13 | Biotronik Mess & Therapieg | System for determining the intracorporeal position of a working catheter |
| JP2002017751A (en) * | 2000-07-06 | 2002-01-22 | Olympus Optical Co Ltd | Surgery navigation device |
| JP2002045372A (en) * | 2000-08-02 | 2002-02-12 | Olympus Optical Co Ltd | Surgical navigation device |
| US6726699B1 (en) | 2000-08-15 | 2004-04-27 | Computer Motion, Inc. | Instrument guide |
| AU2001285071A1 (en) * | 2000-08-17 | 2002-02-25 | John David | Trajectory guide with instrument immobilizer |
| US6823207B1 (en) * | 2000-08-26 | 2004-11-23 | Ge Medical Systems Global Technology Company, Llc | Integrated fluoroscopic surgical navigation and imaging workstation with command protocol |
| US6893447B2 (en) * | 2000-09-24 | 2005-05-17 | Medtronic, Inc. | Surgical reference frame fixation device with cannulated post and method of use |
| US6770082B2 (en) | 2000-09-24 | 2004-08-03 | Medtronic, Inc. | Surgical headframe with soft contact pads for use with a stereotactic system |
| FR2814668B1 (en) | 2000-09-29 | 2003-03-14 | Bertrand Lombard | TRANSMITTER BLOCK HOLDER DEVICE AND RELATED SURGICAL NAVIGATION METHOD AND DEVICE |
| US6860877B1 (en) | 2000-09-29 | 2005-03-01 | Computer Motion, Inc. | Heart stabilizer support arm |
| FR2814669B1 (en) | 2000-09-29 | 2004-01-02 | Bertrand Lombard | SURGICAL NAVIGUATION DEVICE |
| FR2814667B1 (en) | 2000-09-29 | 2002-12-20 | Bertrand Lombard | STEREOTAXIC FRAME, TRANSMITTING BLOCK HOLDER DEVICE AND RELATED SURGICAL NAVIGATION METHOD AND DEVICE |
| US7127081B1 (en) * | 2000-10-12 | 2006-10-24 | Momentum Bilgisayar, Yazilim, Danismanlik, Ticaret, A.S. | Method for tracking motion of a face |
| US6801913B2 (en) * | 2000-10-20 | 2004-10-05 | Canon Kabushiki Kaisha | Medical instrument control system |
| US7066781B2 (en) | 2000-10-20 | 2006-06-27 | Denise Chapman Weston | Children's toy with wireless tag/transponder |
| US6618620B1 (en) | 2000-11-28 | 2003-09-09 | Txsonics Ltd. | Apparatus for controlling thermal dosing in an thermal treatment system |
| WO2002043569A2 (en) * | 2000-11-28 | 2002-06-06 | Intuitive Surgical, Inc. | Endoscopic beating-heart stabilizer and vessel occlusion fastener |
| US6820614B2 (en) | 2000-12-02 | 2004-11-23 | The Bonutti 2003 Trust -A | Tracheal intubination |
| AU3071802A (en) * | 2000-12-08 | 2002-06-18 | Univ Loma Linda Med | Proton beam therapy control system |
| US6666579B2 (en) | 2000-12-28 | 2003-12-23 | Ge Medical Systems Global Technology Company, Llc | Method and apparatus for obtaining and displaying computed tomography images using a fluoroscopy imaging system |
| AU2002248360A1 (en) * | 2001-01-16 | 2002-08-19 | Microdexterity Systems, Inc. | Surgical manipulator |
| US7892243B2 (en) * | 2001-01-16 | 2011-02-22 | Microdexterity Systems, Inc. | Surgical manipulator |
| US20020103430A1 (en) | 2001-01-29 | 2002-08-01 | Hastings Roger N. | Catheter navigation within an MR imaging device |
| DE10105592A1 (en) | 2001-02-06 | 2002-08-08 | Achim Goepferich | Placeholder for drug release in the frontal sinus |
| US20030135204A1 (en) * | 2001-02-15 | 2003-07-17 | Endo Via Medical, Inc. | Robotically controlled medical instrument with a flexible section |
| US7195642B2 (en) | 2001-03-13 | 2007-03-27 | Mckernan Daniel J | Method and apparatus for fixing a graft in a bone tunnel |
| US6517546B2 (en) * | 2001-03-13 | 2003-02-11 | Gregory R. Whittaker | Method and apparatus for fixing a graft in a bone tunnel |
| US7594917B2 (en) | 2001-03-13 | 2009-09-29 | Ethicon, Inc. | Method and apparatus for fixing a graft in a bone tunnel |
| JP2002306509A (en) * | 2001-04-10 | 2002-10-22 | Olympus Optical Co Ltd | Remote operation supporting system |
| US20020165524A1 (en) | 2001-05-01 | 2002-11-07 | Dan Sanchez | Pivot point arm for a robotic system used to perform a surgical procedure |
| CA2348135A1 (en) | 2001-05-17 | 2002-11-17 | Cedara Software Corp. | 3-d navigation for x-ray imaging system |
| JP2002359761A (en) * | 2001-05-31 | 2002-12-13 | Asahi Optical Co Ltd | Cradle for digital camera |
| US7063705B2 (en) | 2001-06-29 | 2006-06-20 | Sdgi Holdings, Inc. | Fluoroscopic locator and registration device |
| US7708741B1 (en) | 2001-08-28 | 2010-05-04 | Marctec, Llc | Method of preparing bones for knee replacement surgery |
| US6728599B2 (en) | 2001-09-07 | 2004-04-27 | Computer Motion, Inc. | Modularity system for computer assisted surgery |
| JP4832679B2 (en) * | 2001-09-11 | 2011-12-07 | オリンパス株式会社 | Microscope system |
| FR2831793A1 (en) | 2001-09-28 | 2003-05-09 | Bertrand Lombard | MOUTHPIECE FOR SURGICAL NAVIGATION DEVICE |
| FR2831795B1 (en) | 2001-09-28 | 2005-02-04 | Bertrand Lombard | ORAL PIECE FOR SURGICAL NAVIGATION DEVICE |
| ATE387892T1 (en) * | 2001-10-10 | 2008-03-15 | Brainlab Ag | MEDICAL INSTRUMENT WITH TOUCH SENSITIVE TIP |
| DE10151398B4 (en) * | 2001-10-18 | 2005-03-17 | Schaerer Mayfield USA, Inc., Cincinnati | Device for adapting surgical instruments as a pointing device |
| US7959860B2 (en) * | 2001-10-22 | 2011-06-14 | Faries Jr Durward I | System and method of detecting fluid and leaks in thermal treatment system basins |
| US6810881B2 (en) | 2001-10-22 | 2004-11-02 | O.R. Solutions, Inc. | Medical solution thermal treatment system and method of controlling system operation in accordance with detection of solution and leaks in surgical drape containers |
| US7854230B2 (en) * | 2001-10-22 | 2010-12-21 | O.R. Solutions, Inc. | Heated medical instrument stand with surgical drape and method of detecting fluid and leaks in the stand tray |
| US7347210B2 (en) * | 2001-10-22 | 2008-03-25 | O.R. Solutions, Inc. | Surgical drape with conductor and method of detecting fluid and leaks in thermal treatment system Basins |
| US7418966B2 (en) * | 2001-10-22 | 2008-09-02 | O. R. Solutions, Inc. | Surgical drape and method of detecting fluid and leaks in thermal treatment system basins |
| EP1446989B1 (en) | 2001-10-30 | 2007-03-21 | Loma Linda University Medical Center | Device for aligning a patient for delivering radiotherapy |
| US7587234B2 (en) * | 2001-11-02 | 2009-09-08 | Abbott Cardiovascular Systems Inc. | Method and apparatus for computer modified magnetic resonance imaging |
| GB0127658D0 (en) * | 2001-11-19 | 2002-01-09 | Acrobot Company The Ltd | Apparatus for surgical instrument location |
| GB0127659D0 (en) * | 2001-11-19 | 2002-01-09 | Acrobot Company The Ltd | Apparatus and method for registering the position of a surgical robot |
| US6793653B2 (en) | 2001-12-08 | 2004-09-21 | Computer Motion, Inc. | Multifunctional handle for a medical robotic system |
| US20030131852A1 (en) * | 2001-12-11 | 2003-07-17 | Izi Corporation | Registration and surgical face mask |
| US7020512B2 (en) * | 2002-01-14 | 2006-03-28 | Stereotaxis, Inc. | Method of localizing medical devices |
| DE60318010T2 (en) * | 2002-01-16 | 2008-11-27 | Orthosoft, Inc., Montreal | METHOD AND DEVICE FOR RECONSTRUCTING BONE SURFACES DURING SURGICAL TREATMENT |
| DE10202091B4 (en) * | 2002-01-21 | 2005-09-08 | Siemens Ag | Device for determining a coordinate transformation |
| US20030210812A1 (en) * | 2002-02-26 | 2003-11-13 | Ali Khamene | Apparatus and method for surgical navigation |
| US6741883B2 (en) | 2002-02-28 | 2004-05-25 | Houston Stereotactic Concepts, Inc. | Audible feedback from positional guidance systems |
| US20030220557A1 (en) * | 2002-03-01 | 2003-11-27 | Kevin Cleary | Image guided liver interventions based on magnetic tracking of internal organ motion |
| US11202676B2 (en) | 2002-03-06 | 2021-12-21 | Mako Surgical Corp. | Neural monitor-based dynamic haptics |
| US8010180B2 (en) | 2002-03-06 | 2011-08-30 | Mako Surgical Corp. | Haptic guidance system and method |
| US7206627B2 (en) | 2002-03-06 | 2007-04-17 | Z-Kat, Inc. | System and method for intra-operative haptic planning of a medical procedure |
| US8996169B2 (en) | 2011-12-29 | 2015-03-31 | Mako Surgical Corp. | Neural monitor-based dynamic haptics |
| JP2003296757A (en) * | 2002-03-29 | 2003-10-17 | Canon Inc | Information processing method and device |
| US20070066396A1 (en) | 2002-04-05 | 2007-03-22 | Denise Chapman Weston | Retail methods for providing an interactive product to a consumer |
| US6967566B2 (en) | 2002-04-05 | 2005-11-22 | Creative Kingdoms, Llc | Live-action interactive adventure game |
| EP1376870A1 (en) * | 2002-06-19 | 2004-01-02 | Senstronic, S.A. | Proximity switch with indicating means and its method of use |
| FI117886B (en) * | 2002-07-29 | 2007-04-13 | Nexstim Oy | Position indicator frame and method for supporting a position indicator frame |
| ATE349944T1 (en) * | 2002-07-31 | 2007-01-15 | Olympus Corp | ENDOSCOPE |
| US7674184B2 (en) | 2002-08-01 | 2010-03-09 | Creative Kingdoms, Llc | Interactive water attraction and quest game |
| US20040176751A1 (en) * | 2002-08-14 | 2004-09-09 | Endovia Medical, Inc. | Robotic medical instrument system |
| US6892090B2 (en) * | 2002-08-19 | 2005-05-10 | Surgical Navigation Technologies, Inc. | Method and apparatus for virtual endoscopy |
| US7704260B2 (en) | 2002-09-17 | 2010-04-27 | Medtronic, Inc. | Low profile instrument immobilizer |
| US7166114B2 (en) * | 2002-09-18 | 2007-01-23 | Stryker Leibinger Gmbh & Co Kg | Method and system for calibrating a surgical tool and adapter thereof |
| US8317816B2 (en) | 2002-09-30 | 2012-11-27 | Acclarent, Inc. | Balloon catheters and methods for treating paranasal sinuses |
| US8052695B2 (en) * | 2002-10-11 | 2011-11-08 | Ge Medical Systems Global Technology Company Llc | Adjustable instruments for use with an electromagnetic localizer |
| US7869861B2 (en) * | 2002-10-25 | 2011-01-11 | Howmedica Leibinger Inc. | Flexible tracking article and method of using the same |
| EP1504712B1 (en) * | 2002-10-29 | 2009-12-02 | Olympus Corporation | Endoscope information processor and processing method |
| US7636596B2 (en) * | 2002-12-20 | 2009-12-22 | Medtronic, Inc. | Organ access device and method |
| US8088067B2 (en) | 2002-12-23 | 2012-01-03 | Insightec Ltd. | Tissue aberration corrections in ultrasound therapy |
| US6822244B2 (en) | 2003-01-02 | 2004-11-23 | Loma Linda University Medical Center | Configuration management and retrieval system for proton beam therapy system |
| US8355773B2 (en) * | 2003-01-21 | 2013-01-15 | Aesculap Ag | Recording localization device tool positional parameters |
| US7492930B2 (en) * | 2003-02-04 | 2009-02-17 | Aesculap Ag | Method and apparatus for capturing information associated with a surgical procedure performed using a localization device |
| WO2004069040A2 (en) * | 2003-02-04 | 2004-08-19 | Z-Kat, Inc. | Method and apparatus for computer assistance with intramedullary nail procedure |
| EP1605810A2 (en) * | 2003-02-04 | 2005-12-21 | Z-Kat, Inc. | Computer-assisted knee replacement apparatus and method |
| US7896889B2 (en) * | 2003-02-20 | 2011-03-01 | Medtronic, Inc. | Trajectory guide with angled or patterned lumens or height adjustment |
| US7559935B2 (en) * | 2003-02-20 | 2009-07-14 | Medtronic, Inc. | Target depth locators for trajectory guide for introducing an instrument |
| US20070055142A1 (en) * | 2003-03-14 | 2007-03-08 | Webler William E | Method and apparatus for image guided position tracking during percutaneous procedures |
| US9446319B2 (en) | 2003-03-25 | 2016-09-20 | Mq Gaming, Llc | Interactive gaming toy |
| US7028387B1 (en) | 2003-03-26 | 2006-04-18 | Advanced Neuromodulation Systems, Inc. | Method of making a miniaturized positional assembly |
| US20060281991A1 (en) * | 2003-05-09 | 2006-12-14 | Fitzpatrick J M | Fiducial marker holder system for surgery |
| US7611462B2 (en) | 2003-05-22 | 2009-11-03 | Insightec-Image Guided Treatment Ltd. | Acoustic beam forming in phased arrays including large numbers of transducer elements |
| US20040243207A1 (en) * | 2003-05-30 | 2004-12-02 | Olson Donald R. | Medical implant systems |
| US20050033117A1 (en) * | 2003-06-02 | 2005-02-10 | Olympus Corporation | Object observation system and method of controlling object observation system |
| US7831295B2 (en) * | 2003-06-05 | 2010-11-09 | Aesculap Ag & Co. Kg | Localization device cross check |
| US20050020909A1 (en) * | 2003-07-10 | 2005-01-27 | Moctezuma De La Barrera Jose Luis | Display device for surgery and method for using the same |
| CA2473963A1 (en) * | 2003-07-14 | 2005-01-14 | Sunnybrook And Women's College Health Sciences Centre | Optical image-based position tracking for magnetic resonance imaging |
| US8150495B2 (en) | 2003-08-11 | 2012-04-03 | Veran Medical Technologies, Inc. | Bodily sealants and methods and apparatus for image-guided delivery of same |
| US7398116B2 (en) | 2003-08-11 | 2008-07-08 | Veran Medical Technologies, Inc. | Methods, apparatuses, and systems useful in conducting image guided interventions |
| ATE547048T1 (en) | 2003-08-12 | 2012-03-15 | Univ Loma Linda Med | MODULAR PATIENT SUPPORT SYSTEM |
| CA2535121C (en) | 2003-08-12 | 2021-03-23 | Loma Linda University Medical Center | Patient positioning system for radiation therapy system |
| US8064985B2 (en) * | 2003-09-12 | 2011-11-22 | Ge Medical Systems Global Technology Company | System and method for determining the position of a flexible instrument used in a tracking system |
| US20050062469A1 (en) * | 2003-09-23 | 2005-03-24 | Anderson Peter Traneus | System and method for hemisphere disambiguation in electromagnetic tracking systems |
| US8354837B2 (en) * | 2003-09-24 | 2013-01-15 | Ge Medical Systems Global Technology Company Llc | System and method for electromagnetic tracking operable with multiple coil architectures |
| US7651506B2 (en) * | 2003-10-02 | 2010-01-26 | University Of Florida Research Foundation, Inc. | Frameless stereotactic guidance of medical procedures |
| US7862570B2 (en) | 2003-10-03 | 2011-01-04 | Smith & Nephew, Inc. | Surgical positioners |
| US20050085723A1 (en) * | 2003-10-04 | 2005-04-21 | Joel Huebner | Radiolucent medical devices with radiopaque markers |
| CA2538126A1 (en) * | 2003-10-06 | 2005-05-06 | Smith & Nephew, Inc. | Modular navigated portal |
| DE10346678A1 (en) * | 2003-10-08 | 2005-05-12 | Siemens Ag | Endoscopy device comprising an endoscopy capsule or an endoscopy head with an image recording device and imaging method for such an endoscopy device |
| WO2005032390A1 (en) * | 2003-10-09 | 2005-04-14 | Ap Technologies Sa | Robot-assisted medical treatment device |
| US7764985B2 (en) | 2003-10-20 | 2010-07-27 | Smith & Nephew, Inc. | Surgical navigation system component fault interfaces and related processes |
| US7197170B2 (en) | 2003-11-10 | 2007-03-27 | M2S, Inc. | Anatomical visualization and measurement system |
| ES2362491T3 (en) | 2003-11-14 | 2011-07-06 | SMITH & NEPHEW, INC. | ADJUSTABLE SURGICAL CUTTING SYSTEMS. |
| US7015859B2 (en) * | 2003-11-14 | 2006-03-21 | General Electric Company | Electromagnetic tracking system and method using a three-coil wireless transmitter |
| US20050247169A1 (en) * | 2003-11-26 | 2005-11-10 | Faries Durward I Jr | Fastening system and method of fastening objects with enhanced security |
| FR2862861B1 (en) | 2003-11-28 | 2006-12-22 | Ge Med Sys Global Tech Co Llc | POSITIONING OBJECTS FOR THE ACQUISITION OF IMAGES |
| US7873400B2 (en) * | 2003-12-10 | 2011-01-18 | Stryker Leibinger Gmbh & Co. Kg. | Adapter for surgical navigation trackers |
| US7771436B2 (en) * | 2003-12-10 | 2010-08-10 | Stryker Leibinger Gmbh & Co. Kg. | Surgical navigation tracker, system and method |
| US7083611B2 (en) * | 2003-12-19 | 2006-08-01 | Marc S. Lemchen | Method and apparatus for providing facial rejuvenation treatments |
| US7350373B1 (en) | 2003-12-23 | 2008-04-01 | O.R. Solutions, Inc. | Surgical disk drape and method of dislodging surgical slush within thermal treatment system basins |
| US20050154279A1 (en) * | 2003-12-31 | 2005-07-14 | Wenguang Li | System and method for registering an image with a representation of a probe |
| US20050154282A1 (en) * | 2003-12-31 | 2005-07-14 | Wenguang Li | System and method for registering an image with a representation of a probe |
| US7966058B2 (en) * | 2003-12-31 | 2011-06-21 | General Electric Company | System and method for registering an image with a representation of a probe |
| US20050154286A1 (en) * | 2004-01-02 | 2005-07-14 | Neason Curtis G. | System and method for receiving and displaying information pertaining to a patient |
| US20050154285A1 (en) * | 2004-01-02 | 2005-07-14 | Neason Curtis G. | System and method for receiving and displaying information pertaining to a patient |
| CA2553368A1 (en) * | 2004-01-16 | 2005-08-11 | Smith & Nephew, Inc. | Computer-assisted ligament balancing in total knee arthroplasty |
| US20050197569A1 (en) * | 2004-01-22 | 2005-09-08 | Mccombs Daniel | Methods, systems, and apparatuses for providing patient-mounted surgical navigational sensors |
| US20060036162A1 (en) * | 2004-02-02 | 2006-02-16 | Ramin Shahidi | Method and apparatus for guiding a medical instrument to a subsurface target site in a patient |
| US20050267353A1 (en) * | 2004-02-04 | 2005-12-01 | Joel Marquart | Computer-assisted knee replacement apparatus and method |
| EP1722848A1 (en) * | 2004-02-13 | 2006-11-22 | Medtronic, Inc. | Methods and apparatus for securing a therapy delivery device within a burr hole |
| US7668285B2 (en) * | 2004-02-16 | 2010-02-23 | Kabushiki Kaisha Toshiba | X-ray computed tomographic apparatus and image processing apparatus |
| US8046050B2 (en) * | 2004-03-05 | 2011-10-25 | Biosense Webster, Inc. | Position sensing system for orthopedic applications |
| CN100441143C (en) * | 2004-02-18 | 2008-12-10 | 皇家飞利浦电子股份有限公司 | Correction of measured values for a magnetic localization device |
| US7403811B2 (en) * | 2004-03-01 | 2008-07-22 | Scimed Life Systems, Inc. | Method of catheter tracking using image information |
| US20070073306A1 (en) * | 2004-03-08 | 2007-03-29 | Ryan Lakin | Cutting block for surgical navigation |
| US7811294B2 (en) * | 2004-03-08 | 2010-10-12 | Mediguide Ltd. | Automatic guidewire maneuvering system and method |
| US20060098010A1 (en) * | 2004-03-09 | 2006-05-11 | Jeff Dwyer | Anatomical visualization and measurement system |
| US20050209524A1 (en) * | 2004-03-10 | 2005-09-22 | General Electric Company | System and method for receiving and storing information pertaining to a patient |
| US7671302B1 (en) | 2004-03-23 | 2010-03-02 | O. R. Solutions, Inc. | Thermal treatment system instrument rack and method of selectively thermally treating medical instrument portions |
| US7728262B1 (en) | 2004-03-23 | 2010-06-01 | O.R. Solutions, Inc. | Thermal treatment system instrument rack and method of selectively thermally treating medical instrument portions |
| US20050228251A1 (en) * | 2004-03-30 | 2005-10-13 | General Electric Company | System and method for displaying a three-dimensional image of an organ or structure inside the body |
| US20050228252A1 (en) * | 2004-04-02 | 2005-10-13 | General Electric Company | Electrophysiology system and method |
| US20050222509A1 (en) * | 2004-04-02 | 2005-10-06 | General Electric Company | Electrophysiology system and method |
| US9554691B2 (en) | 2004-04-21 | 2017-01-31 | Acclarent, Inc. | Endoscopic methods and devices for transnasal procedures |
| US9089258B2 (en) | 2004-04-21 | 2015-07-28 | Acclarent, Inc. | Endoscopic methods and devices for transnasal procedures |
| US20070167682A1 (en) | 2004-04-21 | 2007-07-19 | Acclarent, Inc. | Endoscopic methods and devices for transnasal procedures |
| US8747389B2 (en) | 2004-04-21 | 2014-06-10 | Acclarent, Inc. | Systems for treating disorders of the ear, nose and throat |
| US8932276B1 (en) | 2004-04-21 | 2015-01-13 | Acclarent, Inc. | Shapeable guide catheters and related methods |
| US7410480B2 (en) | 2004-04-21 | 2008-08-12 | Acclarent, Inc. | Devices and methods for delivering therapeutic substances for the treatment of sinusitis and other disorders |
| US8702626B1 (en) | 2004-04-21 | 2014-04-22 | Acclarent, Inc. | Guidewires for performing image guided procedures |
| US20190314620A1 (en) | 2004-04-21 | 2019-10-17 | Acclarent, Inc. | Apparatus and methods for dilating and modifying ostia of paranasal sinuses and other intranasal or paranasal structures |
| US9101384B2 (en) | 2004-04-21 | 2015-08-11 | Acclarent, Inc. | Devices, systems and methods for diagnosing and treating sinusitis and other disorders of the ears, Nose and/or throat |
| US8146400B2 (en) | 2004-04-21 | 2012-04-03 | Acclarent, Inc. | Endoscopic methods and devices for transnasal procedures |
| US8764729B2 (en) | 2004-04-21 | 2014-07-01 | Acclarent, Inc. | Frontal sinus spacer |
| US20070208252A1 (en) * | 2004-04-21 | 2007-09-06 | Acclarent, Inc. | Systems and methods for performing image guided procedures within the ear, nose, throat and paranasal sinuses |
| US7462175B2 (en) | 2004-04-21 | 2008-12-09 | Acclarent, Inc. | Devices, systems and methods for treating disorders of the ear, nose and throat |
| US7559925B2 (en) | 2006-09-15 | 2009-07-14 | Acclarent Inc. | Methods and devices for facilitating visualization in a surgical environment |
| US20060004323A1 (en) | 2004-04-21 | 2006-01-05 | Exploramed Nc1, Inc. | Apparatus and methods for dilating and modifying ostia of paranasal sinuses and other intranasal or paranasal structures |
| US7361168B2 (en) | 2004-04-21 | 2008-04-22 | Acclarent, Inc. | Implantable device and methods for delivering drugs and other substances to treat sinusitis and other disorders |
| US7720521B2 (en) * | 2004-04-21 | 2010-05-18 | Acclarent, Inc. | Methods and devices for performing procedures within the ear, nose, throat and paranasal sinuses |
| US7654997B2 (en) | 2004-04-21 | 2010-02-02 | Acclarent, Inc. | Devices, systems and methods for diagnosing and treating sinusitus and other disorders of the ears, nose and/or throat |
| WO2005104978A1 (en) | 2004-04-21 | 2005-11-10 | Smith & Nephew, Inc. | Computer-aided methods, systems, and apparatuses for shoulder arthroplasty |
| US7419497B2 (en) | 2004-04-21 | 2008-09-02 | Acclarent, Inc. | Methods for treating ethmoid disease |
| US9351750B2 (en) | 2004-04-21 | 2016-05-31 | Acclarent, Inc. | Devices and methods for treating maxillary sinus disease |
| US9399121B2 (en) | 2004-04-21 | 2016-07-26 | Acclarent, Inc. | Systems and methods for transnasal dilation of passageways in the ear, nose or throat |
| US10188413B1 (en) | 2004-04-21 | 2019-01-29 | Acclarent, Inc. | Deflectable guide catheters and related methods |
| US20060063973A1 (en) | 2004-04-21 | 2006-03-23 | Acclarent, Inc. | Methods and apparatus for treating disorders of the ear, nose and throat |
| US8894614B2 (en) | 2004-04-21 | 2014-11-25 | Acclarent, Inc. | Devices, systems and methods useable for treating frontal sinusitis |
| US7803150B2 (en) | 2004-04-21 | 2010-09-28 | Acclarent, Inc. | Devices, systems and methods useable for treating sinusitis |
| US7711405B2 (en) * | 2004-04-28 | 2010-05-04 | Siemens Corporation | Method of registering pre-operative high field closed magnetic resonance images with intra-operative low field open interventional magnetic resonance images |
| WO2005119578A2 (en) * | 2004-06-02 | 2005-12-15 | Medical Metrx Solutions, Inc. | Anatomical visualization and measurement system |
| US20050288574A1 (en) * | 2004-06-23 | 2005-12-29 | Thornton Thomas M | Wireless (disposable) fiducial based registration and EM distoration based surface registration |
| US7073508B2 (en) | 2004-06-25 | 2006-07-11 | Loma Linda University Medical Center | Method and device for registration and immobilization |
| US8409099B2 (en) | 2004-08-26 | 2013-04-02 | Insightec Ltd. | Focused ultrasound system for surrounding a body tissue mass and treatment method |
| US20060063998A1 (en) * | 2004-09-21 | 2006-03-23 | Von Jako Ron | Navigation and visualization of an access needle system |
| US20060064005A1 (en) * | 2004-09-23 | 2006-03-23 | Innovative Spinal Technologies | System and method for externally controlled surgical navigation |
| US9216015B2 (en) | 2004-10-28 | 2015-12-22 | Vycor Medical, Inc. | Apparatus and methods for performing brain surgery |
| US7702137B2 (en) | 2004-11-10 | 2010-04-20 | M2S, Inc. | Anatomical visualization and measurement system |
| EP1815796A4 (en) * | 2004-11-17 | 2009-10-28 | Hitachi Medical Corp | Ultrasonograph and ultrasonic image display method |
| DE102004058122A1 (en) * | 2004-12-02 | 2006-07-13 | Siemens Ag | Medical image registration aid for landmarks by computerized and photon emission tomographies, comprises permeable radioactive substance is filled with the emission tomography as radiation permeable containers, a belt and patient body bowl |
| US20060200025A1 (en) * | 2004-12-02 | 2006-09-07 | Scott Elliott | Systems, methods, and apparatus for automatic software flow using instrument detection during computer-aided surgery |
| US7497863B2 (en) * | 2004-12-04 | 2009-03-03 | Medtronic, Inc. | Instrument guiding stage apparatus and method for using same |
| US7744606B2 (en) * | 2004-12-04 | 2010-06-29 | Medtronic, Inc. | Multi-lumen instrument guide |
| US7976518B2 (en) | 2005-01-13 | 2011-07-12 | Corpak Medsystems, Inc. | Tubing assembly and signal generator placement control device and method for use with catheter guidance systems |
| CA2594863A1 (en) * | 2005-01-14 | 2006-07-20 | Micronix Pty Ltd | Guiding insert assembly for a catheter used with a catheter position guidance system |
| US20060161051A1 (en) * | 2005-01-18 | 2006-07-20 | Lauralan Terrill-Grisoni | Method of computer-assisted ligament balancing and component placement in total knee arthroplasty |
| WO2006081409A2 (en) * | 2005-01-28 | 2006-08-03 | Massachusetts General Hospital | Guidance and insertion system |
| US7623250B2 (en) * | 2005-02-04 | 2009-11-24 | Stryker Leibinger Gmbh & Co. Kg. | Enhanced shape characterization device and method |
| JP2006218129A (en) * | 2005-02-10 | 2006-08-24 | Olympus Corp | Surgery supporting system |
| FR2882245B1 (en) * | 2005-02-21 | 2007-05-18 | Gen Electric | METHOD FOR DETERMINING THE 3D DISPLACEMENT OF A PATIENT POSITIONED ON A TABLE OF AN IMAGING DEVICE |
| AU2006216653B2 (en) | 2005-02-22 | 2012-03-15 | Smith & Nephew, Inc. | In-line milling system |
| GB0504172D0 (en) * | 2005-03-01 | 2005-04-06 | King S College London | Surgical planning |
| DE102005013851B4 (en) * | 2005-03-24 | 2014-11-27 | Siemens Aktiengesellschaft | Method for supporting an examination by means of an imaging diagnostic device |
| US9421019B2 (en) * | 2005-04-07 | 2016-08-23 | Omnilife Science, Inc. | Robotic guide assembly for use in computer-aided surgery |
| US7318001B2 (en) | 2005-05-03 | 2008-01-08 | Cnv Technologies, Llc | Method and apparatus for collecting data for detecting and locating disturbances |
| JP2008539903A (en) * | 2005-05-06 | 2008-11-20 | リージェンツ オブ ザ ユニバーシティ オブ ミネソタ | Wirelessly coupled magnetic resonance coil |
| US8208988B2 (en) * | 2005-05-13 | 2012-06-26 | General Electric Company | System and method for controlling a medical imaging device |
| US8097003B2 (en) * | 2005-05-13 | 2012-01-17 | Boston Scientific Scimed, Inc. | Endoscopic apparatus with integrated variceal ligation device |
| US10555775B2 (en) | 2005-05-16 | 2020-02-11 | Intuitive Surgical Operations, Inc. | Methods and system for performing 3-D tool tracking by fusion of sensor and/or camera derived data during minimally invasive robotic surgery |
| EP1887946A2 (en) | 2005-06-06 | 2008-02-20 | The Board Of Regents, The University Of Texas System | Oct using spectrally resolved bandwidth |
| JP5741885B2 (en) * | 2005-06-09 | 2015-07-01 | ナヴィスイス エージー | System and method for non-contact determination and measurement of the spatial position and / or orientation of an object, in particular a medical instrument calibration and test method including a pattern or structure relating to a medical instrument |
| US8951225B2 (en) | 2005-06-10 | 2015-02-10 | Acclarent, Inc. | Catheters with non-removable guide members useable for treatment of sinusitis |
| US20060287583A1 (en) | 2005-06-17 | 2006-12-21 | Pool Cover Corporation | Surgical access instruments for use with delicate tissues |
| US20070016039A1 (en) | 2005-06-21 | 2007-01-18 | Insightec-Image Guided Treatment Ltd. | Controlled, non-linear focused ultrasound treatment |
| US20070016008A1 (en) * | 2005-06-23 | 2007-01-18 | Ryan Schoenefeld | Selective gesturing input to a surgical navigation system |
| WO2006137012A2 (en) * | 2005-06-23 | 2006-12-28 | Philips Intellectual Property & Standards Gmbh | Method and apparatus for inductively measuring the bio-impedance of a user's body |
| US7840256B2 (en) | 2005-06-27 | 2010-11-23 | Biomet Manufacturing Corporation | Image guided tracking array and method |
| US8583220B2 (en) * | 2005-08-02 | 2013-11-12 | Biosense Webster, Inc. | Standardization of catheter-based treatment for atrial fibrillation |
| US7877128B2 (en) * | 2005-08-02 | 2011-01-25 | Biosense Webster, Inc. | Simulation of invasive procedures |
| JP4805633B2 (en) | 2005-08-22 | 2011-11-02 | 任天堂株式会社 | Game operation device |
| US8313379B2 (en) | 2005-08-22 | 2012-11-20 | Nintendo Co., Ltd. | Video game system with wireless modular handheld controller |
| US7927216B2 (en) | 2005-09-15 | 2011-04-19 | Nintendo Co., Ltd. | Video game system with wireless modular handheld controller |
| JP4262726B2 (en) | 2005-08-24 | 2009-05-13 | 任天堂株式会社 | Game controller and game system |
| US8870655B2 (en) | 2005-08-24 | 2014-10-28 | Nintendo Co., Ltd. | Wireless game controllers |
| US8784336B2 (en) | 2005-08-24 | 2014-07-22 | C. R. Bard, Inc. | Stylet apparatuses and methods of manufacture |
| US8308563B2 (en) | 2005-08-30 | 2012-11-13 | Nintendo Co., Ltd. | Game system and storage medium having game program stored thereon |
| US8148666B2 (en) * | 2005-09-01 | 2012-04-03 | Patented Medical Solutions, Llc | Method and apparatus for protecting sterile drapes in surgical thermal treatment systems |
| US8157651B2 (en) | 2005-09-12 | 2012-04-17 | Nintendo Co., Ltd. | Information processing program |
| US20070066881A1 (en) * | 2005-09-13 | 2007-03-22 | Edwards Jerome R | Apparatus and method for image guided accuracy verification |
| EP1924198B1 (en) | 2005-09-13 | 2019-04-03 | Veran Medical Technologies, Inc. | Apparatus for image guided accuracy verification |
| US8038625B2 (en) * | 2005-09-15 | 2011-10-18 | St. Jude Medical, Atrial Fibrillation Division, Inc. | System and method for three-dimensional mapping of electrophysiology information |
| US8229545B2 (en) | 2005-09-15 | 2012-07-24 | St. Jude Medical, Atrial Fibrillation Division, Inc. | System and method for mapping complex fractionated electrogram information |
| US7643862B2 (en) * | 2005-09-15 | 2010-01-05 | Biomet Manufacturing Corporation | Virtual mouse for use in surgical navigation |
| US8114113B2 (en) | 2005-09-23 | 2012-02-14 | Acclarent, Inc. | Multi-conduit balloon catheter |
| US20070078678A1 (en) * | 2005-09-30 | 2007-04-05 | Disilvestro Mark R | System and method for performing a computer assisted orthopaedic surgical procedure |
| US10299871B2 (en) | 2005-09-30 | 2019-05-28 | Restoration Robotics, Inc. | Automated system and method for hair removal |
| US20070078466A1 (en) * | 2005-09-30 | 2007-04-05 | Restoration Robotics, Inc. | Methods for harvesting follicular units using an automated system |
| US7962192B2 (en) | 2005-09-30 | 2011-06-14 | Restoration Robotics, Inc. | Systems and methods for aligning a tool with a desired location or object |
| US7918793B2 (en) * | 2005-10-28 | 2011-04-05 | Biosense Webster, Inc. | Synchronization of ultrasound imaging data with electrical mapping |
| ITMI20052060A1 (en) * | 2005-10-28 | 2007-04-29 | Sintesi S C P A | EQUIPMENT FOR THE MOVEMENT OF SURGICAL ORGANS |
| DE102005053759B4 (en) * | 2005-11-10 | 2010-04-29 | Siemens Ag | Method and device for the wireless transmission of energy from a magnetic coil system to a working capsule |
| US20070129629A1 (en) * | 2005-11-23 | 2007-06-07 | Beauregard Gerald L | System and method for surgical navigation |
| US20070167744A1 (en) * | 2005-11-23 | 2007-07-19 | General Electric Company | System and method for surgical navigation cross-reference to related applications |
| US7711406B2 (en) * | 2005-11-23 | 2010-05-04 | General Electric Company | System and method for detection of electromagnetic radiation by amorphous silicon x-ray detector for metal detection in x-ray imaging |
| JP5087007B2 (en) | 2005-11-23 | 2012-11-28 | インサイテック・リミテッド | Hierarchical switching ultra high density ultrasonic array |
| WO2007064739A2 (en) | 2005-11-29 | 2007-06-07 | Surgi-Vision, Inc. | Mri-guided localization and/or lead placement systems, related methods, devices and computer program products |
| US7640121B2 (en) * | 2005-11-30 | 2009-12-29 | General Electric Company | System and method for disambiguating the phase of a field received from a transmitter in an electromagnetic tracking system |
| US8303505B2 (en) * | 2005-12-02 | 2012-11-06 | Abbott Cardiovascular Systems Inc. | Methods and apparatuses for image guided medical procedures |
| JP5313689B2 (en) * | 2005-12-29 | 2013-10-09 | ギブン イメージング リミテッド | System for determining the position of an in-vivo sensing device and method of operating the system |
| US20070161888A1 (en) * | 2005-12-30 | 2007-07-12 | Sherman Jason T | System and method for registering a bone of a patient with a computer assisted orthopaedic surgery system |
| US7525309B2 (en) * | 2005-12-30 | 2009-04-28 | Depuy Products, Inc. | Magnetic sensor array |
| US20070167741A1 (en) * | 2005-12-30 | 2007-07-19 | Sherman Jason T | Apparatus and method for registering a bone of a patient with a computer assisted orthopaedic surgery system |
| US8862200B2 (en) * | 2005-12-30 | 2014-10-14 | DePuy Synthes Products, LLC | Method for determining a position of a magnetic source |
| US9084556B2 (en) * | 2006-01-19 | 2015-07-21 | Toshiba Medical Systems Corporation | Apparatus for indicating locus of an ultrasonic probe, ultrasonic diagnostic apparatus |
| EP1818651A1 (en) * | 2006-02-10 | 2007-08-15 | Rijksuniversiteit Groningen | System and a method for determining one or more parameters of a source of a potential-energy field |
| US8219177B2 (en) * | 2006-02-16 | 2012-07-10 | Catholic Healthcare West | Method and system for performing invasive medical procedures using a surgical robot |
| US8219178B2 (en) * | 2007-02-16 | 2012-07-10 | Catholic Healthcare West | Method and system for performing invasive medical procedures using a surgical robot |
| WO2007095637A1 (en) * | 2006-02-16 | 2007-08-23 | Catholic Healthcare West (D/B/A St. Joseph's Hospital Medical Center) | System utilizing radio frequency signals for tracking and improving navigation of slender instruments during insertion into the body |
| JP4151982B2 (en) | 2006-03-10 | 2008-09-17 | 任天堂株式会社 | Motion discrimination device and motion discrimination program |
| US7557710B2 (en) * | 2006-03-17 | 2009-07-07 | Med Wave, Llc | System for tracking surgical items in an operating room environment |
| CN102599875B (en) * | 2006-03-22 | 2015-03-11 | 皇家飞利浦电子股份有限公司 | Medical instrument system |
| US8165659B2 (en) | 2006-03-22 | 2012-04-24 | Garrett Sheffer | Modeling method and apparatus for use in surgical navigation |
| GB0605807D0 (en) * | 2006-03-23 | 2006-05-03 | Depuy Int Ltd | A template for use in a surgical procedure |
| EP1998702A2 (en) * | 2006-03-29 | 2008-12-10 | Stryker Corporation | Shielded surgical navigation system that determines the position and orientation of the tracked object with real and virtual dipoles |
| US7471202B2 (en) | 2006-03-29 | 2008-12-30 | General Electric Co. | Conformal coil array for a medical tracking system |
| EP2005208B1 (en) * | 2006-03-31 | 2017-08-16 | Koninklijke Philips N.V. | System for local error compensation in electromagnetic tracking systems |
| US7532997B2 (en) | 2006-04-17 | 2009-05-12 | General Electric Company | Electromagnetic tracking using a discretized numerical field model |
| US8235901B2 (en) | 2006-04-26 | 2012-08-07 | Insightec, Ltd. | Focused ultrasound system with far field tail suppression |
| US7794387B2 (en) | 2006-04-26 | 2010-09-14 | Medtronic, Inc. | Methods and devices for stabilizing tissue |
| US8190389B2 (en) | 2006-05-17 | 2012-05-29 | Acclarent, Inc. | Adapter for attaching electromagnetic image guidance components to a medical device |
| US7988639B2 (en) * | 2006-05-17 | 2011-08-02 | St. Jude Medical, Atrial Fibrillation Division, Inc. | System and method for complex geometry modeling of anatomy using multiple surface models |
| JP2009537229A (en) * | 2006-05-19 | 2009-10-29 | マコ サージカル コーポレーション | Method and apparatus for controlling a haptic device |
| EP2023812B1 (en) * | 2006-05-19 | 2016-01-27 | The Queen's Medical Center | Motion tracking system for real time adaptive imaging and spectroscopy |
| US8635082B2 (en) | 2006-05-25 | 2014-01-21 | DePuy Synthes Products, LLC | Method and system for managing inventories of orthopaedic implants |
| US8125648B2 (en) | 2006-06-05 | 2012-02-28 | Board Of Regents, The University Of Texas System | Polarization-sensitive spectral interferometry |
| US8280483B2 (en) * | 2006-06-14 | 2012-10-02 | Koninklijke Philips Electronics N.V. | Multi-modality medical image viewing |
| US8560047B2 (en) | 2006-06-16 | 2013-10-15 | Board Of Regents Of The University Of Nebraska | Method and apparatus for computer aided surgery |
| DE502006003264D1 (en) * | 2006-06-27 | 2009-05-07 | Brainlab Ag | Medical-technical marker tracking with determination of marker properties |
| US20080033278A1 (en) * | 2006-08-01 | 2008-02-07 | Insightec Ltd. | System and method for tracking medical device using magnetic resonance detection |
| US8040127B2 (en) * | 2006-08-15 | 2011-10-18 | General Electric Company | Multi-sensor distortion mapping method and system |
| US8442619B2 (en) * | 2006-08-30 | 2013-05-14 | General Electric Company | System and method for detecting errors in position tracking systems used for medical applications |
| US8197494B2 (en) | 2006-09-08 | 2012-06-12 | Corpak Medsystems, Inc. | Medical device position guidance system with wireless connectivity between a noninvasive device and an invasive device |
| US9820688B2 (en) | 2006-09-15 | 2017-11-21 | Acclarent, Inc. | Sinus illumination lightwire device |
| US8248414B2 (en) * | 2006-09-18 | 2012-08-21 | Stryker Corporation | Multi-dimensional navigation of endoscopic video |
| US7824328B2 (en) * | 2006-09-18 | 2010-11-02 | Stryker Corporation | Method and apparatus for tracking a surgical instrument during surgery |
| US8248413B2 (en) | 2006-09-18 | 2012-08-21 | Stryker Corporation | Visual navigation system for endoscopic surgery |
| US7945310B2 (en) * | 2006-09-18 | 2011-05-17 | Stryker Corporation | Surgical instrument path computation and display for endoluminal surgery |
| US20080123910A1 (en) * | 2006-09-19 | 2008-05-29 | Bracco Imaging Spa | Method and system for providing accuracy evaluation of image guided surgery |
| US10016148B2 (en) * | 2006-09-27 | 2018-07-10 | General Electric Company | Method and apparatus for correction of multiple EM sensor positions |
| US8543188B2 (en) * | 2006-10-17 | 2013-09-24 | General Electric Company | Method and apparatus for calibrating medical devices |
| US8388546B2 (en) | 2006-10-23 | 2013-03-05 | Bard Access Systems, Inc. | Method of locating the tip of a central venous catheter |
| US7794407B2 (en) | 2006-10-23 | 2010-09-14 | Bard Access Systems, Inc. | Method of locating the tip of a central venous catheter |
| US20080108991A1 (en) * | 2006-11-08 | 2008-05-08 | General Electric Company | Method and apparatus for performing pedicle screw fusion surgery |
| US9320569B2 (en) * | 2006-11-14 | 2016-04-26 | General Electric Company | Systems and methods for implant distance measurement |
| US7671887B2 (en) * | 2006-11-20 | 2010-03-02 | General Electric Company | System and method of navigating a medical instrument |
| US20080118116A1 (en) * | 2006-11-20 | 2008-05-22 | General Electric Company | Systems and methods for tracking a surgical instrument and for conveying tracking information via a network |
| CA2670002C (en) | 2006-11-21 | 2017-03-14 | Loma Linda University Medical Center | Device and method for immobilizing patients for breast radiation therapy |
| US20080132757A1 (en) * | 2006-12-01 | 2008-06-05 | General Electric Company | System and Method for Performing Minimally Invasive Surgery Using a Multi-Channel Catheter |
| US20080139929A1 (en) * | 2006-12-06 | 2008-06-12 | General Electric Company | System and method for tracking an invasive surgical instrument while imaging a patient |
| US8068648B2 (en) * | 2006-12-21 | 2011-11-29 | Depuy Products, Inc. | Method and system for registering a bone of a patient with a computer assisted orthopaedic surgery system |
| US20080177203A1 (en) * | 2006-12-22 | 2008-07-24 | General Electric Company | Surgical navigation planning system and method for placement of percutaneous instrumentation and implants |
| US20080154120A1 (en) * | 2006-12-22 | 2008-06-26 | General Electric Company | Systems and methods for intraoperative measurements on navigated placements of implants |
| US8439687B1 (en) | 2006-12-29 | 2013-05-14 | Acclarent, Inc. | Apparatus and method for simulated insertion and positioning of guidewares and other interventional devices |
| US7508195B2 (en) * | 2007-01-18 | 2009-03-24 | General Electric Company | Anti-distortion electromagnetic sensor method and system |
| US7573258B2 (en) * | 2007-01-18 | 2009-08-11 | General Electric Company | Coil arrangement for electromagnetic tracker method and system |
| JP5127242B2 (en) | 2007-01-19 | 2013-01-23 | 任天堂株式会社 | Acceleration data processing program and game program |
| US20080183064A1 (en) * | 2007-01-30 | 2008-07-31 | General Electric Company | Multi-sensor distortion detection method and system |
| EP1952779B1 (en) * | 2007-02-01 | 2012-04-04 | BrainLAB AG | Method and system for Identification of medical instruments |
| US7782046B2 (en) | 2007-02-05 | 2010-08-24 | General Electric Company | Electromagnetic tracking method and system |
| WO2008103383A1 (en) * | 2007-02-20 | 2008-08-28 | Gildenberg Philip L | Videotactic and audiotactic assisted surgical methods and procedures |
| US7950306B2 (en) | 2007-02-23 | 2011-05-31 | Microdexterity Systems, Inc. | Manipulator |
| US8249689B2 (en) * | 2007-02-23 | 2012-08-21 | General Electric Company | Coil arrangement for electromagnetic tracking method and system |
| WO2008111070A2 (en) * | 2007-03-12 | 2008-09-18 | David Tolkowsky | Devices and methods for performing medical procedures in tree-like luminal structures |
| US20080228065A1 (en) * | 2007-03-13 | 2008-09-18 | Viswanathan Raju R | System and Method for Registration of Localization and Imaging Systems for Navigational Control of Medical Devices |
| US8821511B2 (en) * | 2007-03-15 | 2014-09-02 | General Electric Company | Instrument guide for use with a surgical navigation system |
| US7902817B2 (en) * | 2007-03-26 | 2011-03-08 | General Electric Company | Electromagnetic tracking method and system |
| DE102007014828A1 (en) * | 2007-03-28 | 2008-10-09 | Siemens Ag | Detecting device for detecting an object in at least two dimensions by means of X-rays in response to a body signal and method |
| WO2008124787A2 (en) | 2007-04-09 | 2008-10-16 | Acclarent, Inc. | Ethmoidotomy system and implantable spacer devices having therapeutic substance delivery capability for treatment of paranasal sinusitis |
| US8301226B2 (en) * | 2007-04-24 | 2012-10-30 | Medtronic, Inc. | Method and apparatus for performing a navigated procedure |
| US8734466B2 (en) | 2007-04-25 | 2014-05-27 | Medtronic, Inc. | Method and apparatus for controlled insertion and withdrawal of electrodes |
| US20090012509A1 (en) * | 2007-04-24 | 2009-01-08 | Medtronic, Inc. | Navigated Soft Tissue Penetrating Laser System |
| US8311611B2 (en) * | 2007-04-24 | 2012-11-13 | Medtronic, Inc. | Method for performing multiple registrations in a navigated procedure |
| US9289270B2 (en) * | 2007-04-24 | 2016-03-22 | Medtronic, Inc. | Method and apparatus for performing a navigated procedure |
| US8108025B2 (en) * | 2007-04-24 | 2012-01-31 | Medtronic, Inc. | Flexible array for use in navigated surgery |
| US8118757B2 (en) | 2007-04-30 | 2012-02-21 | Acclarent, Inc. | Methods and devices for ostium measurement |
| US8485199B2 (en) | 2007-05-08 | 2013-07-16 | Acclarent, Inc. | Methods and devices for protecting nasal turbinate during surgery |
| US8428690B2 (en) | 2007-05-16 | 2013-04-23 | General Electric Company | Intracardiac echocardiography image reconstruction in combination with position tracking system |
| US8989842B2 (en) | 2007-05-16 | 2015-03-24 | General Electric Company | System and method to register a tracking system with intracardiac echocardiography (ICE) imaging system |
| US8527032B2 (en) | 2007-05-16 | 2013-09-03 | General Electric Company | Imaging system and method of delivery of an instrument to an imaged subject |
| US8364242B2 (en) * | 2007-05-17 | 2013-01-29 | General Electric Company | System and method of combining ultrasound image acquisition with fluoroscopic image acquisition |
| US8934961B2 (en) | 2007-05-18 | 2015-01-13 | Biomet Manufacturing, Llc | Trackable diagnostic scope apparatus and methods of use |
| US8175677B2 (en) * | 2007-06-07 | 2012-05-08 | MRI Interventions, Inc. | MRI-guided medical interventional systems and methods |
| US20090003528A1 (en) | 2007-06-19 | 2009-01-01 | Sankaralingam Ramraj | Target location by tracking of imaging device |
| US20080319491A1 (en) * | 2007-06-19 | 2008-12-25 | Ryan Schoenefeld | Patient-matched surgical component and methods of use |
| US9883818B2 (en) | 2007-06-19 | 2018-02-06 | Accuray Incorporated | Fiducial localization |
| EP2626030A3 (en) * | 2007-08-14 | 2017-03-08 | Koninklijke Philips N.V. | Robotic instrument systems and methods utilizing optical fiber sensors |
| DE102007043366A1 (en) * | 2007-09-12 | 2009-03-19 | Degudent Gmbh | Method for determining the position of an intraoral measuring device |
| CA2700523A1 (en) | 2007-09-24 | 2009-04-02 | Surgivision, Inc. | Mri-guided medical interventional systems and methods |
| US8315689B2 (en) | 2007-09-24 | 2012-11-20 | MRI Interventions, Inc. | MRI surgical systems for real-time visualizations using MRI image data and predefined data of surgical tools |
| US7912662B2 (en) * | 2007-09-24 | 2011-03-22 | General Electric Company | System and method for improving the distortion tolerance of an electromagnetic tracking system |
| US7834621B2 (en) * | 2007-09-25 | 2010-11-16 | General Electric Company | Electromagnetic tracking employing scalar-magnetometer |
| US8265949B2 (en) | 2007-09-27 | 2012-09-11 | Depuy Products, Inc. | Customized patient surgical plan |
| ES2802126T3 (en) | 2007-09-30 | 2021-01-15 | Depuy Products Inc | Patient Specific Custom Orthopedic Surgical Instrument |
| US8251908B2 (en) | 2007-10-01 | 2012-08-28 | Insightec Ltd. | Motion compensated image-guided focused ultrasound therapy system |
| US20090085559A1 (en) * | 2007-10-02 | 2009-04-02 | General Electric Company | System and method for minimizing electromagnetic field distortion in an electromagnetic tracking system |
| US8391952B2 (en) * | 2007-10-11 | 2013-03-05 | General Electric Company | Coil arrangement for an electromagnetic tracking system |
| US8781555B2 (en) | 2007-11-26 | 2014-07-15 | C. R. Bard, Inc. | System for placement of a catheter including a signal-generating stylet |
| ES2651898T3 (en) | 2007-11-26 | 2018-01-30 | C.R. Bard Inc. | Integrated system for intravascular catheter placement |
| US10751509B2 (en) | 2007-11-26 | 2020-08-25 | C. R. Bard, Inc. | Iconic representations for guidance of an indwelling medical device |
| US10524691B2 (en) | 2007-11-26 | 2020-01-07 | C. R. Bard, Inc. | Needle assembly including an aligned magnetic element |
| US9521961B2 (en) | 2007-11-26 | 2016-12-20 | C. R. Bard, Inc. | Systems and methods for guiding a medical instrument |
| US8849382B2 (en) | 2007-11-26 | 2014-09-30 | C. R. Bard, Inc. | Apparatus and display methods relating to intravascular placement of a catheter |
| US9649048B2 (en) | 2007-11-26 | 2017-05-16 | C. R. Bard, Inc. | Systems and methods for breaching a sterile field for intravascular placement of a catheter |
| US10449330B2 (en) | 2007-11-26 | 2019-10-22 | C. R. Bard, Inc. | Magnetic element-equipped needle assemblies |
| US9636031B2 (en) | 2007-11-26 | 2017-05-02 | C.R. Bard, Inc. | Stylets for use with apparatus for intravascular placement of a catheter |
| US10206821B2 (en) | 2007-12-20 | 2019-02-19 | Acclarent, Inc. | Eustachian tube dilation balloon with ventilation path |
| ES2595366T3 (en) * | 2008-01-09 | 2016-12-29 | Stryker European Holdings I, Llc | Computer-assisted stereotactic surgery system based on a three-dimensional visualization |
| US8571637B2 (en) * | 2008-01-21 | 2013-10-29 | Biomet Manufacturing, Llc | Patella tracking method and apparatus for use in surgical navigation |
| JP5669340B2 (en) | 2008-01-23 | 2015-02-12 | シスメックス株式会社 | Sample analyzer and program for sample analyzer |
| US8478382B2 (en) | 2008-02-11 | 2013-07-02 | C. R. Bard, Inc. | Systems and methods for positioning a catheter |
| US20090209888A1 (en) * | 2008-02-18 | 2009-08-20 | Seyed Hessam Khatami | Spine Wheel |
| EP2247253A4 (en) | 2008-02-22 | 2015-08-05 | Univ Loma Linda Med | Systems and methods for characterizing spatial distortion in 3d imaging systems |
| US9179985B2 (en) * | 2008-03-03 | 2015-11-10 | Koninklijke Philips N.V. | Biopsy guidance by electromagnetic tracking and photonic needle |
| US20090224047A1 (en) * | 2008-03-05 | 2009-09-10 | Konica Minolta Systems Laboratory, Inc. | Contactless Scan Position Orientation Sensing |
| US8182432B2 (en) | 2008-03-10 | 2012-05-22 | Acclarent, Inc. | Corewire design and construction for medical devices |
| US9168173B2 (en) * | 2008-04-04 | 2015-10-27 | Truevision Systems, Inc. | Apparatus and methods for performing enhanced visually directed procedures under low ambient light conditions |
| US8789534B2 (en) * | 2008-04-09 | 2014-07-29 | Patented Medical Solutions, Llc | Method and apparatus for warming medical solutions in a thermal treatment system employing a removable basin |
| EP2108328B2 (en) * | 2008-04-09 | 2020-08-26 | Brainlab AG | Image-based control method for medicinal devices |
| US8260578B2 (en) * | 2008-05-19 | 2012-09-04 | The Procter & Gamble Company | Method of determining the dynamic location of a protection |
| US8185354B2 (en) * | 2008-05-19 | 2012-05-22 | The Procter & Gamble Company | Method of determining the dynamic location of a protection device |
| EP2123220A1 (en) * | 2008-05-20 | 2009-11-25 | Oticon A/S | A probe and coil fixed thereto for establishing the spatial location of a probe body and a method of fixedly position a magnetic generating means to a probe body and a system for obtaining geometrical data related to a cavity |
| MX2011001099A (en) | 2008-07-30 | 2011-03-15 | Acclarent Inc | Paranasal ostium finder devices and methods. |
| ES2525525T3 (en) | 2008-08-22 | 2014-12-26 | C.R. Bard, Inc. | Catheter assembly that includes ECG and magnetic sensor assemblies |
| JP5584687B2 (en) | 2008-09-18 | 2014-09-03 | アクラレント インコーポレイテッド | Method and apparatus for treating ear, nose and throat disorders |
| US8086298B2 (en) * | 2008-09-29 | 2011-12-27 | Civco Medical Instruments Co., Inc. | EM tracking systems for use with ultrasound and other imaging modalities |
| US8437833B2 (en) | 2008-10-07 | 2013-05-07 | Bard Access Systems, Inc. | Percutaneous magnetic gastrostomy |
| US9226798B2 (en) | 2008-10-10 | 2016-01-05 | Truevision Systems, Inc. | Real-time surgical reference indicium apparatus and methods for surgical applications |
| US10117721B2 (en) * | 2008-10-10 | 2018-11-06 | Truevision Systems, Inc. | Real-time surgical reference guides and methods for surgical applications |
| CA2742260A1 (en) * | 2008-10-30 | 2010-05-27 | Troy D. Payner | Systems and methods for guiding a medical instrument |
| US9033958B2 (en) * | 2008-11-11 | 2015-05-19 | Perception Raisonnement Action En Medecine | Surgical robotic system |
| US8425424B2 (en) | 2008-11-19 | 2013-04-23 | Inightee Ltd. | Closed-loop clot lysis |
| DE102009007986A1 (en) * | 2009-02-07 | 2010-08-12 | Radl, Bernd, Dr. | Device for illuminating a surgical field of a sterile operating room |
| US9173717B2 (en) * | 2009-02-20 | 2015-11-03 | Truevision Systems, Inc. | Real-time surgical reference indicium apparatus and methods for intraocular lens implantation |
| US8504139B2 (en) | 2009-03-10 | 2013-08-06 | Medtronic Xomed, Inc. | Navigating a surgical instrument |
| US9226689B2 (en) | 2009-03-10 | 2016-01-05 | Medtronic Xomed, Inc. | Flexible circuit sheet |
| US9226688B2 (en) | 2009-03-10 | 2016-01-05 | Medtronic Xomed, Inc. | Flexible circuit assemblies |
| US20100241155A1 (en) | 2009-03-20 | 2010-09-23 | Acclarent, Inc. | Guide system with suction |
| US8435290B2 (en) | 2009-03-31 | 2013-05-07 | Acclarent, Inc. | System and method for treatment of non-ventilating middle ear by providing a gas pathway through the nasopharynx |
| US7978742B1 (en) | 2010-03-24 | 2011-07-12 | Corning Incorporated | Methods for operating diode lasers |
| US8617073B2 (en) | 2009-04-17 | 2013-12-31 | Insightec Ltd. | Focusing ultrasound into the brain through the skull by utilizing both longitudinal and shear waves |
| US20100275718A1 (en) * | 2009-04-29 | 2010-11-04 | Microdexterity Systems, Inc. | Manipulator |
| US8308043B2 (en) * | 2009-05-19 | 2012-11-13 | Covidien Lp | Recognition of interchangeable component of a device |
| US9259290B2 (en) | 2009-06-08 | 2016-02-16 | MRI Interventions, Inc. | MRI-guided surgical systems with proximity alerts |
| US9445734B2 (en) | 2009-06-12 | 2016-09-20 | Bard Access Systems, Inc. | Devices and methods for endovascular electrography |
| ES2745861T3 (en) | 2009-06-12 | 2020-03-03 | Bard Access Systems Inc | Apparatus, computer-aided data-processing algorithm, and computer storage medium for positioning an endovascular device in or near the heart |
| US9532724B2 (en) | 2009-06-12 | 2017-01-03 | Bard Access Systems, Inc. | Apparatus and method for catheter navigation using endovascular energy mapping |
| JP2012529977A (en) | 2009-06-16 | 2012-11-29 | エムアールアイ・インターヴェンションズ,インコーポレイテッド | MRI guidance device and MRI guidance intervention system capable of tracking the device in near real time and generating a dynamic visualization of the device |
| US9623266B2 (en) | 2009-08-04 | 2017-04-18 | Insightec Ltd. | Estimation of alignment parameters in magnetic-resonance-guided ultrasound focusing |
| US9289154B2 (en) | 2009-08-19 | 2016-03-22 | Insightec Ltd. | Techniques for temperature measurement and corrections in long-term magnetic resonance thermometry |
| WO2011024074A2 (en) | 2009-08-26 | 2011-03-03 | Insightec Ltd. | Asymmetric phased-array ultrasound transducer |
| WO2011023232A1 (en) | 2009-08-27 | 2011-03-03 | Brainlab Ag | Disposable and radiolucent reference array for optical tracking |
| EP2298223A1 (en) | 2009-09-21 | 2011-03-23 | Stryker Leibinger GmbH & Co. KG | Technique for registering image data of an object |
| EP2483710A4 (en) | 2009-10-01 | 2016-04-27 | Univ Loma Linda Med | Ion induced impact ionization detector and uses thereof |
| WO2011044421A1 (en) | 2009-10-08 | 2011-04-14 | C. R. Bard, Inc. | Spacers for use with an ultrasound probe |
| US10639008B2 (en) | 2009-10-08 | 2020-05-05 | C. R. Bard, Inc. | Support and cover structures for an ultrasound probe head |
| EP2489034B1 (en) | 2009-10-14 | 2016-11-30 | Insightec Ltd. | Mapping ultrasound transducers |
| US8784443B2 (en) * | 2009-10-20 | 2014-07-22 | Truevision Systems, Inc. | Real-time surgical reference indicium apparatus and methods for astigmatism correction |
| US9314189B2 (en) * | 2009-11-06 | 2016-04-19 | Biotronik Crm Patent Ag | Extracorporeal physiological measurement device |
| US8368401B2 (en) | 2009-11-10 | 2013-02-05 | Insightec Ltd. | Techniques for correcting measurement artifacts in magnetic resonance thermometry |
| US8376938B2 (en) * | 2009-11-20 | 2013-02-19 | Ethicon Endo-Surgery, Inc. | Discrete flexion head for single port device |
| US8363919B2 (en) | 2009-11-25 | 2013-01-29 | Imaging Sciences International Llc | Marker identification and processing in x-ray images |
| US9082182B2 (en) * | 2009-11-25 | 2015-07-14 | Dental Imaging Technologies Corporation | Extracting patient motion vectors from marker positions in x-ray images |
| US9826942B2 (en) * | 2009-11-25 | 2017-11-28 | Dental Imaging Technologies Corporation | Correcting and reconstructing x-ray images using patient motion vectors extracted from marker positions in x-ray images |
| US8180130B2 (en) * | 2009-11-25 | 2012-05-15 | Imaging Sciences International Llc | Method for X-ray marker localization in 3D space in the presence of motion |
| US9082036B2 (en) * | 2009-11-25 | 2015-07-14 | Dental Imaging Technologies Corporation | Method for accurate sub-pixel localization of markers on X-ray images |
| US9082177B2 (en) * | 2009-11-25 | 2015-07-14 | Dental Imaging Technologies Corporation | Method for tracking X-ray markers in serial CT projection images |
| US8435174B2 (en) * | 2009-12-11 | 2013-05-07 | Ethicon Endo-Surgery, Inc. | Methods and devices for accessing a body cavity |
| US8231570B2 (en) * | 2009-12-11 | 2012-07-31 | Ethicon Endo-Surgery, Inc. | Inverted conical expandable retractor |
| US8357088B2 (en) * | 2009-12-11 | 2013-01-22 | Ethicon Endo-Surgery, Inc. | Methods and devices for providing access into a body cavity |
| US8500633B2 (en) * | 2009-12-11 | 2013-08-06 | Ethicon Endo-Surgery, Inc. | Methods and devices for providing surgical access through tissue to a surgical site |
| US8444557B2 (en) * | 2009-12-11 | 2013-05-21 | Ethicon Endo-Surgery, Inc. | Methods and devices for providing access through tissue to a surgical site |
| US8353873B2 (en) * | 2009-12-11 | 2013-01-15 | Ethicon Endo-Surgery, Inc. | Methods and devices for providing access through tissue to a surgical site |
| US8282546B2 (en) * | 2009-12-11 | 2012-10-09 | Ethicon Endo-Surgery, Inc. | Inverted conical expandable retractor with coil spring |
| US8414483B2 (en) * | 2009-12-11 | 2013-04-09 | Ethicon Endo-Surgery, Inc. | Methods and devices for providing access into a body cavity |
| US8517932B2 (en) * | 2009-12-11 | 2013-08-27 | Ethicon Endo-Surgery, Inc. | Methods and devices for providing access through tissue to a surgical site |
| US8460186B2 (en) * | 2009-12-11 | 2013-06-11 | Ethicon Endo-Surgery, Inc. | Methods and devices for providing access through tissue to a surgical site |
| US8348831B2 (en) * | 2009-12-15 | 2013-01-08 | Zhejiang University | Device and method for computer simulated marking targeting biopsy |
| US8600480B2 (en) | 2009-12-31 | 2013-12-03 | Mediguide Ltd. | System and method for assessing interference to a signal caused by a magnetic field |
| JP5650248B2 (en) | 2010-02-01 | 2015-01-07 | コビディエン エルピー | Region expansion algorithm |
| CN102821679B (en) | 2010-02-02 | 2016-04-27 | C·R·巴德股份有限公司 | For the apparatus and method that catheter navigation and end are located |
| US20110213342A1 (en) * | 2010-02-26 | 2011-09-01 | Ashok Burton Tripathi | Real-time Virtual Indicium Apparatus and Methods for Guiding an Implant into an Eye |
| WO2011106797A1 (en) | 2010-02-28 | 2011-09-01 | Osterhout Group, Inc. | Projection triggering through an external marker in an augmented reality eyepiece |
| US20120194553A1 (en) * | 2010-02-28 | 2012-08-02 | Osterhout Group, Inc. | Ar glasses with sensor and user action based control of external devices with feedback |
| US10180572B2 (en) | 2010-02-28 | 2019-01-15 | Microsoft Technology Licensing, Llc | AR glasses with event and user action control of external applications |
| US20150309316A1 (en) | 2011-04-06 | 2015-10-29 | Microsoft Technology Licensing, Llc | Ar glasses with predictive control of external device based on event input |
| US20120249797A1 (en) | 2010-02-28 | 2012-10-04 | Osterhout Group, Inc. | Head-worn adaptive display |
| US10588647B2 (en) * | 2010-03-01 | 2020-03-17 | Stryker European Holdings I, Llc | Computer assisted surgery system |
| US9216257B2 (en) * | 2010-03-25 | 2015-12-22 | Medtronic, Inc. | Method and apparatus for guiding an external needle to an implantable device |
| US9339601B2 (en) * | 2010-03-25 | 2016-05-17 | Medtronic, Inc. | Method and apparatus for guiding an external needle to an implantable device |
| US8483802B2 (en) * | 2010-03-25 | 2013-07-09 | Medtronic, Inc. | Method and apparatus for guiding an external needle to an implantable device |
| US8475407B2 (en) * | 2010-03-25 | 2013-07-02 | Medtronic, Inc. | Method and apparatus for guiding an external needle to an implantable device |
| US8932237B2 (en) | 2010-04-28 | 2015-01-13 | Insightec, Ltd. | Efficient ultrasound focusing |
| US9852727B2 (en) | 2010-04-28 | 2017-12-26 | Insightec, Ltd. | Multi-segment ultrasound transducers |
| EP3563788A1 (en) | 2010-04-30 | 2019-11-06 | Medtronic Xomed, Inc. | Navigated malleable surgical instrument |
| JP2013530028A (en) | 2010-05-04 | 2013-07-25 | パスファインダー セラピューティクス,インコーポレイテッド | System and method for abdominal surface matching using pseudo features |
| ES2778041T3 (en) | 2010-05-28 | 2020-08-07 | Bard Inc C R | Apparatus for use with needle insertion guidance system |
| EP2912999B1 (en) | 2010-05-28 | 2022-06-29 | C. R. Bard, Inc. | Apparatus for use with needle insertion guidance system |
| US9414980B2 (en) * | 2010-06-08 | 2016-08-16 | Panasonic Intellectual Property Management Co., Ltd. | Bed, and combining method and separating method of bed |
| EP2584965B1 (en) * | 2010-06-28 | 2016-04-13 | Koninklijke Philips N.V. | Real-time quality control of em calibration |
| ES2665268T3 (en) | 2010-07-15 | 2018-04-25 | The Cleveland Clinic Foundation | Classification of impacts from sensor data |
| AU2010357460B2 (en) | 2010-07-16 | 2013-10-31 | Stryker European Operations Holdings Llc | Surgical targeting system and method |
| WO2012024577A2 (en) | 2010-08-20 | 2012-02-23 | C.R. Bard, Inc. | Reconfirmation of ecg-assisted catheter tip placement |
| EP2605693B1 (en) | 2010-08-20 | 2019-11-06 | Veran Medical Technologies, Inc. | Apparatus for four dimensional soft tissue navigation |
| EP2700375B1 (en) | 2010-09-02 | 2018-10-24 | Ecolab USA Inc. | Selective thermal treatment of medical instrument portions with thermal treatment system instrument holder |
| US9155492B2 (en) | 2010-09-24 | 2015-10-13 | Acclarent, Inc. | Sinus illumination lightwire device |
| US8702592B2 (en) * | 2010-09-30 | 2014-04-22 | David Allan Langlois | System and method for inhibiting injury to a patient during laparoscopic surgery |
| US11231787B2 (en) | 2010-10-06 | 2022-01-25 | Nuvasive, Inc. | Imaging system and method for use in surgical and interventional medical procedures |
| US9785246B2 (en) | 2010-10-06 | 2017-10-10 | Nuvasive, Inc. | Imaging system and method for use in surgical and interventional medical procedures |
| US8526700B2 (en) | 2010-10-06 | 2013-09-03 | Robert E. Isaacs | Imaging system and method for surgical and interventional medical procedures |
| US8603078B2 (en) | 2010-10-13 | 2013-12-10 | Ethicon Endo-Surgery, Inc. | Methods and devices for guiding and supporting surgical instruments |
| US9981148B2 (en) | 2010-10-22 | 2018-05-29 | Insightec, Ltd. | Adaptive active cooling during focused ultrasound treatment |
| US8801693B2 (en) | 2010-10-29 | 2014-08-12 | C. R. Bard, Inc. | Bioimpedance-assisted placement of a medical device |
| EP2654559B1 (en) * | 2010-12-23 | 2021-11-24 | Bard Access Systems, Inc. | System to guide a rigid instrument |
| US9921712B2 (en) | 2010-12-29 | 2018-03-20 | Mako Surgical Corp. | System and method for providing substantially stable control of a surgical tool |
| US9119655B2 (en) | 2012-08-03 | 2015-09-01 | Stryker Corporation | Surgical manipulator capable of controlling a surgical instrument in multiple modes |
| US20130019374A1 (en) | 2011-01-04 | 2013-01-24 | Schwartz Alan N | Gel-based seals and fixation devices and associated systems and methods |
| US11045246B1 (en) | 2011-01-04 | 2021-06-29 | Alan N. Schwartz | Apparatus for effecting feedback of vaginal cavity physiology |
| US10617374B2 (en) | 2011-01-28 | 2020-04-14 | Medtronic Navigation, Inc. | Method and apparatus for image-based navigation |
| US9974501B2 (en) | 2011-01-28 | 2018-05-22 | Medtronic Navigation, Inc. | Method and apparatus for image-based navigation |
| US10492868B2 (en) | 2011-01-28 | 2019-12-03 | Medtronic Navigation, Inc. | Method and apparatus for image-based navigation |
| US9585619B2 (en) | 2011-02-18 | 2017-03-07 | The Cleveland Clinic Foundation | Registration of head impact detection assembly |
| IT1404499B1 (en) * | 2011-02-23 | 2013-11-22 | Grande Nicola Maria Ditta Individuale | NAVIGATION SYSTEM FOR DENTAL AND MAXILLOFACIAL INTERVENTIONS. |
| WO2012149548A2 (en) * | 2011-04-29 | 2012-11-01 | The Johns Hopkins University | System and method for tracking and navigation |
| US20120289830A1 (en) * | 2011-05-10 | 2012-11-15 | General Electric Company | Method and ultrasound imaging system for image-guided procedures |
| US9220510B2 (en) | 2011-06-15 | 2015-12-29 | Perception Raisonnement Action En Medecine | System and method for bone preparation for an implant |
| US9498231B2 (en) | 2011-06-27 | 2016-11-22 | Board Of Regents Of The University Of Nebraska | On-board tool tracking system and methods of computer assisted surgery |
| CN103764061B (en) | 2011-06-27 | 2017-03-08 | 内布拉斯加大学评议会 | Tracing system and Computer Aided Surgery method that instrument carries |
| US11911117B2 (en) | 2011-06-27 | 2024-02-27 | Board Of Regents Of The University Of Nebraska | On-board tool tracking system and methods of computer assisted surgery |
| AU2012278809B2 (en) | 2011-07-06 | 2016-09-29 | C.R. Bard, Inc. | Needle length determination and calibration for insertion guidance system |
| US20130030363A1 (en) | 2011-07-29 | 2013-01-31 | Hansen Medical, Inc. | Systems and methods utilizing shape sensing fibers |
| USD724745S1 (en) | 2011-08-09 | 2015-03-17 | C. R. Bard, Inc. | Cap for an ultrasound probe |
| USD699359S1 (en) | 2011-08-09 | 2014-02-11 | C. R. Bard, Inc. | Ultrasound probe head |
| US8617176B2 (en) | 2011-08-24 | 2013-12-31 | Depuy Mitek, Llc | Cross pinning guide devices and methods |
| US9606209B2 (en) | 2011-08-26 | 2017-03-28 | Kineticor, Inc. | Methods, systems, and devices for intra-scan motion correction |
| CA2847182C (en) | 2011-09-02 | 2020-02-11 | Stryker Corporation | Surgical instrument including a cutting accessory extending from a housing and actuators that establish the position of the cutting accessory relative to the housing |
| US9028441B2 (en) | 2011-09-08 | 2015-05-12 | Corpak Medsystems, Inc. | Apparatus and method used with guidance system for feeding and suctioning |
| US20130249907A1 (en) * | 2011-09-12 | 2013-09-26 | Medical Modeling Inc., a Colorado Corporaiton | Fiducial system to facilitate co-registration and image pixel calibration of multimodal data |
| CN103797512B (en) * | 2011-09-13 | 2018-10-16 | 皇家飞利浦有限公司 | Automatic between robot and image online is registrated |
| WO2013044944A1 (en) * | 2011-09-28 | 2013-04-04 | Brainlab Ag | Self-localizing medical device |
| US9750486B2 (en) | 2011-10-25 | 2017-09-05 | Medtronic Navigation, Inc. | Trackable biopsy needle |
| JP6219835B2 (en) | 2011-10-28 | 2017-10-25 | ディスィジョン サイエンシズ インターナショナル コーポレーション | Spread spectrum coded waveforms in ultrasound imaging |
| US9211107B2 (en) | 2011-11-07 | 2015-12-15 | C. R. Bard, Inc. | Ruggedized ultrasound hydrogel insert |
| US9107737B2 (en) | 2011-11-21 | 2015-08-18 | Alan Schwartz | Goggles with facial conforming eyepieces |
| US9138165B2 (en) | 2012-02-22 | 2015-09-22 | Veran Medical Technologies, Inc. | Systems, methods and devices for forming respiratory-gated point cloud for four dimensional soft tissue navigation |
| CN104244861B (en) * | 2012-03-23 | 2017-09-08 | 皇家飞利浦有限公司 | It is a kind of to be used for the guiding system of the guide instrument in body |
| WO2013173810A2 (en) * | 2012-05-17 | 2013-11-21 | Schwartz Alan N | Localization of the parathyroid |
| US8750568B2 (en) | 2012-05-22 | 2014-06-10 | Covidien Lp | System and method for conformal ablation planning |
| US9439627B2 (en) | 2012-05-22 | 2016-09-13 | Covidien Lp | Planning system and navigation system for an ablation procedure |
| US9439623B2 (en) | 2012-05-22 | 2016-09-13 | Covidien Lp | Surgical planning system and navigation system |
| US9498182B2 (en) | 2012-05-22 | 2016-11-22 | Covidien Lp | Systems and methods for planning and navigation |
| US9439622B2 (en) | 2012-05-22 | 2016-09-13 | Covidien Lp | Surgical navigation system |
| WO2013182224A1 (en) * | 2012-06-05 | 2013-12-12 | Brainlab Ag | Improving the accuracy of navigating a medical device |
| EP2861153A4 (en) | 2012-06-15 | 2016-10-19 | Bard Inc C R | Apparatus and methods for detection of a removable cap on an ultrasound probe |
| US20130338493A1 (en) * | 2012-06-19 | 2013-12-19 | Covidien Lp | Surgical devices, systems and methods for highlighting and measuring regions of interest |
| WO2013192598A1 (en) * | 2012-06-21 | 2013-12-27 | Excelsius Surgical, L.L.C. | Surgical robot platform |
| US9033903B2 (en) | 2012-07-12 | 2015-05-19 | The Trustees Of The Stevens Institute Of Technology | Tri-axial electro-goniometer for spinal motion, associated system and methods |
| US9226796B2 (en) | 2012-08-03 | 2016-01-05 | Stryker Corporation | Method for detecting a disturbance as an energy applicator of a surgical instrument traverses a cutting path |
| US9820818B2 (en) | 2012-08-03 | 2017-11-21 | Stryker Corporation | System and method for controlling a surgical manipulator based on implant parameters |
| CN104519798B (en) | 2012-08-03 | 2018-03-23 | 皇家飞利浦有限公司 | The superposition for the device location dependence drawn for route |
| KR102397265B1 (en) | 2012-08-03 | 2022-05-12 | 스트리커 코포레이션 | Systems and methods for robotic surgery |
| US20140051983A1 (en) * | 2012-08-15 | 2014-02-20 | Tobias Schroeder | Electromagnetic instrument tracking system with metal distortion detection and unlimited hemisphere operation |
| US9552660B2 (en) | 2012-08-30 | 2017-01-24 | Truevision Systems, Inc. | Imaging system and methods displaying a fused multidimensional reconstructed image |
| EP2900156B1 (en) | 2012-09-27 | 2017-07-12 | Stryker European Holdings I, LLC | Rotational position determination |
| US9993273B2 (en) | 2013-01-16 | 2018-06-12 | Mako Surgical Corp. | Bone plate and tracking device using a bone plate for attaching to a patient's anatomy |
| AU2014207502B2 (en) * | 2013-01-16 | 2018-10-18 | Stryker Corporation | Navigation systems and methods for indicating line-of-sight errors |
| US10327708B2 (en) | 2013-01-24 | 2019-06-25 | Kineticor, Inc. | Systems, devices, and methods for tracking and compensating for patient motion during a medical imaging scan |
| US9305365B2 (en) | 2013-01-24 | 2016-04-05 | Kineticor, Inc. | Systems, devices, and methods for tracking moving targets |
| WO2014120734A1 (en) | 2013-02-01 | 2014-08-07 | Kineticor, Inc. | Motion tracking system for real time adaptive motion compensation in biomedical imaging |
| KR102101435B1 (en) | 2013-03-13 | 2020-04-17 | 스트리커 코포레이션 | System for arranging objects in an operating room in preparation for surgical procedures |
| US9057600B2 (en) | 2013-03-13 | 2015-06-16 | Hansen Medical, Inc. | Reducing incremental measurement sensor error |
| CA2897873A1 (en) | 2013-03-13 | 2014-10-09 | Stryker Corporation | Systems and methods for establishing virtual constraint boundaries |
| US10188831B2 (en) | 2013-03-14 | 2019-01-29 | Angiodynamics, Inc. | Systems and methods for catheter tip placement using ECG |
| US10105149B2 (en) | 2013-03-15 | 2018-10-23 | Board Of Regents Of The University Of Nebraska | On-board tool tracking system and methods of computer assisted surgery |
| US9271663B2 (en) | 2013-03-15 | 2016-03-01 | Hansen Medical, Inc. | Flexible instrument localization from both remote and elongation sensors |
| US9014851B2 (en) | 2013-03-15 | 2015-04-21 | Hansen Medical, Inc. | Systems and methods for tracking robotically controlled medical instruments |
| US9629684B2 (en) | 2013-03-15 | 2017-04-25 | Acclarent, Inc. | Apparatus and method for treatment of ethmoid sinusitis |
| US9433437B2 (en) | 2013-03-15 | 2016-09-06 | Acclarent, Inc. | Apparatus and method for treatment of ethmoid sinusitis |
| US9854991B2 (en) | 2013-03-15 | 2018-01-02 | Medtronic Navigation, Inc. | Integrated navigation array |
| US10278729B2 (en) | 2013-04-26 | 2019-05-07 | Medtronic Xomed, Inc. | Medical device and its construction |
| EP3003118B1 (en) * | 2013-06-05 | 2021-11-10 | Check-Cap Ltd. | Position estimation of imaging capsule in gastrointestinal tract |
| US9844359B2 (en) | 2013-09-13 | 2017-12-19 | Decision Sciences Medical Company, LLC | Coherent spread-spectrum coded waveforms in synthetic aperture image formation |
| CA2924230C (en) | 2013-09-18 | 2020-03-31 | iMIRGE Medical INC. | Optical targeting and visusalization of trajectories |
| US10433911B2 (en) | 2013-09-18 | 2019-10-08 | iMIRGE Medical INC. | Optical targeting and visualization of trajectories |
| US20160267659A1 (en) * | 2013-10-25 | 2016-09-15 | Brainlab Ag | Method and device for co-registering a medical 3d image and a spatial reference |
| DE102013112375A1 (en) * | 2013-11-11 | 2015-05-13 | Aesculap Ag | Surgical referencing device, surgical navigation system and method |
| US20150202073A1 (en) * | 2014-01-21 | 2015-07-23 | Aktina Corp. | Head and cervical spine position articulating device |
| US20150216541A1 (en) * | 2014-02-03 | 2015-08-06 | Arthrex, Inc. | Pointing device and drilling tool |
| CN105979868B (en) | 2014-02-06 | 2020-03-10 | C·R·巴德股份有限公司 | Systems and methods for guidance and placement of intravascular devices |
| WO2015142933A1 (en) * | 2014-03-17 | 2015-09-24 | Intuitive Surgical Operations, Inc. | Guided setup for teleoperated medical device |
| KR102450087B1 (en) | 2014-03-17 | 2022-10-06 | 인튜어티브 서지컬 오퍼레이션즈 인코포레이티드 | Automated structure with pre-established arm positions in a teleoperated medical system |
| GB2524498A (en) * | 2014-03-24 | 2015-09-30 | Scopis Gmbh | Electromagnetic navigation system for microscopic surgery |
| US20150282734A1 (en) | 2014-04-08 | 2015-10-08 | Timothy Schweikert | Medical device placement system and a method for its use |
| US20150305650A1 (en) | 2014-04-23 | 2015-10-29 | Mark Hunter | Apparatuses and methods for endobronchial navigation to and confirmation of the location of a target tissue and percutaneous interception of the target tissue |
| US20150305612A1 (en) | 2014-04-23 | 2015-10-29 | Mark Hunter | Apparatuses and methods for registering a real-time image feed from an imaging device to a steerable catheter |
| JP2017515593A (en) | 2014-05-13 | 2017-06-15 | ビコール メディカル,インコーポレイティド | Guide system attachment for a surgical introducer |
| EP3443925B1 (en) | 2014-05-14 | 2021-02-24 | Stryker European Holdings I, LLC | Processor arrangement for tracking the position of a work target |
| US10471278B2 (en) | 2014-06-26 | 2019-11-12 | University Of Florida Research Foundation, Incorporated | Cranial alignment device for use in intracranial stereotactic surgery |
| CN106232010B (en) | 2014-07-02 | 2020-03-31 | 柯惠有限合伙公司 | System and method for detecting trachea |
| US9603668B2 (en) | 2014-07-02 | 2017-03-28 | Covidien Lp | Dynamic 3D lung map view for tool navigation inside the lung |
| US9754367B2 (en) | 2014-07-02 | 2017-09-05 | Covidien Lp | Trachea marking |
| US20160000414A1 (en) | 2014-07-02 | 2016-01-07 | Covidien Lp | Methods for marking biopsy location |
| AU2015283946B2 (en) | 2014-07-02 | 2019-09-12 | Covidien Lp | Real-time automatic registration feedback |
| US9770216B2 (en) | 2014-07-02 | 2017-09-26 | Covidien Lp | System and method for navigating within the lung |
| CN106659453B (en) | 2014-07-02 | 2020-05-26 | 柯惠有限合伙公司 | System and method for segmenting lungs |
| WO2016014718A1 (en) | 2014-07-23 | 2016-01-28 | Kineticor, Inc. | Systems, devices, and methods for tracking and compensating for patient motion during a medical imaging scan |
| US9950194B2 (en) | 2014-09-09 | 2018-04-24 | Mevion Medical Systems, Inc. | Patient positioning system |
| CN105476634B (en) * | 2014-09-15 | 2019-02-22 | 西门子(深圳)磁共振有限公司 | Imaging device and positioning device |
| US10154239B2 (en) | 2014-12-30 | 2018-12-11 | Onpoint Medical, Inc. | Image-guided surgery with surface reconstruction and augmented reality visualization |
| US10973584B2 (en) | 2015-01-19 | 2021-04-13 | Bard Access Systems, Inc. | Device and method for vascular access |
| KR20230169485A (en) | 2015-02-25 | 2023-12-15 | 디시전 사이선씨즈 메디컬 컴패니, 엘엘씨 | Acoustic signal transmission couplants and coupling mediums |
| US10349890B2 (en) | 2015-06-26 | 2019-07-16 | C. R. Bard, Inc. | Connector interface for ECG-based catheter positioning system |
| US9943247B2 (en) | 2015-07-28 | 2018-04-17 | The University Of Hawai'i | Systems, devices, and methods for detecting false movements for motion correction during a medical imaging scan |
| US10986990B2 (en) | 2015-09-24 | 2021-04-27 | Covidien Lp | Marker placement |
| JP6755308B2 (en) | 2015-10-08 | 2020-09-16 | ディスィジョン サイエンシズ メディカル カンパニー,エルエルシー | Acoustic orthopedic tracking system and method |
| US10709352B2 (en) | 2015-10-27 | 2020-07-14 | Covidien Lp | Method of using lung airway carina locations to improve ENB registration |
| US20170119474A1 (en) * | 2015-10-28 | 2017-05-04 | Endochoice, Inc. | Device and Method for Tracking the Position of an Endoscope within a Patient's Body |
| WO2017091479A1 (en) | 2015-11-23 | 2017-06-01 | Kineticor, Inc. | Systems, devices, and methods for tracking and compensating for patient motion during a medical imaging scan |
| JP6876065B2 (en) * | 2015-12-14 | 2021-05-26 | ニューヴェイジヴ,インコーポレイテッド | 3D visualization during surgery with reduced radiation |
| CN113925610A (en) | 2015-12-31 | 2022-01-14 | 史赛克公司 | System and method for performing a procedure on a patient at a target site defined by a virtual object |
| US11000207B2 (en) | 2016-01-29 | 2021-05-11 | C. R. Bard, Inc. | Multiple coil system for tracking a medical device |
| US10151606B1 (en) | 2016-02-24 | 2018-12-11 | Ommo Technologies, Inc. | Tracking position and movement using a magnetic field |
| CA3016604A1 (en) | 2016-03-12 | 2017-09-21 | Philipp K. Lang | Devices and methods for surgery |
| IL245339A (en) | 2016-04-21 | 2017-10-31 | Rani Ben Yishai | Method and system for registration verification |
| US10537395B2 (en) | 2016-05-26 | 2020-01-21 | MAKO Surgical Group | Navigation tracker with kinematic connector assembly |
| WO2017214103A1 (en) * | 2016-06-06 | 2017-12-14 | Temple University-Of The Commonwealth System Of Higher Education | Magnetometer surgical device |
| US11191506B2 (en) * | 2016-07-08 | 2021-12-07 | Ricoh Company, Ltd. | Diagnosis support system, diagnosis support apparatus, and recording medium |
| US20180092698A1 (en) * | 2016-10-04 | 2018-04-05 | WortheeMed, Inc. | Enhanced Reality Medical Guidance Systems and Methods of Use |
| US10152786B2 (en) | 2016-10-11 | 2018-12-11 | Biosense Webster (Israel) Ltd. | Registration of a magnetic tracking system with an imaging device |
| US10631935B2 (en) * | 2016-10-25 | 2020-04-28 | Biosense Webster (Israel) Ltd. | Head registration using a personalized gripper |
| US10376258B2 (en) | 2016-11-07 | 2019-08-13 | Vycor Medical, Inc. | Surgical introducer with guidance system receptacle |
| US10543016B2 (en) | 2016-11-07 | 2020-01-28 | Vycor Medical, Inc. | Surgical introducer with guidance system receptacle |
| US10529088B2 (en) | 2016-12-02 | 2020-01-07 | Gabriel Fine | Automatically determining orientation and position of medically invasive devices via image processing |
| WO2018112025A1 (en) | 2016-12-16 | 2018-06-21 | Mako Surgical Corp. | Techniques for modifying tool operation in a surgical robotic system based on comparing actual and commanded states of the tool relative to a surgical site |
| KR101863574B1 (en) * | 2016-12-29 | 2018-06-01 | 경북대학교 산학협력단 | Application method to fluoroscopy in laser guidance system, recording medium and laser guidance system including calibration tool for performing the method |
| US11751944B2 (en) | 2017-01-16 | 2023-09-12 | Philipp K. Lang | Optical guidance for surgical, medical, and dental procedures |
| FR3063006A1 (en) | 2017-02-20 | 2018-08-24 | Pytheas Navigation | SURGICAL ORIENTATION SYSTEM USING BONE GEOMETRY FOR REPEATABLE POSITIONING |
| US10537350B2 (en) | 2017-03-28 | 2020-01-21 | Biosense Webster (Israel) Ltd. | Medical device having a reusable position sensor |
| US10905497B2 (en) | 2017-04-21 | 2021-02-02 | Clearpoint Neuro, Inc. | Surgical navigation systems |
| US10299880B2 (en) | 2017-04-24 | 2019-05-28 | Truevision Systems, Inc. | Stereoscopic visualization camera and platform |
| US10917543B2 (en) | 2017-04-24 | 2021-02-09 | Alcon Inc. | Stereoscopic visualization camera and integrated robotics platform |
| US11083537B2 (en) | 2017-04-24 | 2021-08-10 | Alcon Inc. | Stereoscopic camera with fluorescence visualization |
| ES2848830T3 (en) | 2017-04-27 | 2021-08-12 | Bard Access Systems Inc | Guiding system to guide the insertion of a needle into the body of a patient comprising a magnetization system for needle assemblies |
| US10699448B2 (en) | 2017-06-29 | 2020-06-30 | Covidien Lp | System and method for identifying, marking and navigating to a target using real time two dimensional fluoroscopic data |
| AU2018214021A1 (en) * | 2017-08-10 | 2019-02-28 | Biosense Webster (Israel) Ltd. | Method and apparatus for performing facial registration |
| US11801114B2 (en) | 2017-09-11 | 2023-10-31 | Philipp K. Lang | Augmented reality display for vascular and other interventions, compensation for cardiac and respiratory motion |
| CN109745119B (en) * | 2017-11-06 | 2023-09-29 | 艾博纽诺股份公司 | Device and method for calibrating and measuring target points for a cerebral nerve navigator |
| WO2019110084A1 (en) * | 2017-12-04 | 2019-06-13 | Diamontech Gmbh | Device and method for analysing a substance |
| WO2019148154A1 (en) | 2018-01-29 | 2019-08-01 | Lang Philipp K | Augmented reality guidance for orthopedic and other surgical procedures |
| US11224392B2 (en) | 2018-02-01 | 2022-01-18 | Covidien Lp | Mapping disease spread |
| US11191594B2 (en) | 2018-05-25 | 2021-12-07 | Mako Surgical Corp. | Versatile tracking arrays for a navigation system and methods of recovering registration using the same |
| US10276289B1 (en) | 2018-06-01 | 2019-04-30 | Ommo Technologies, Inc. | Rotating a permanent magnet in a position detection system |
| US11051829B2 (en) | 2018-06-26 | 2021-07-06 | DePuy Synthes Products, Inc. | Customized patient-specific orthopaedic surgical instrument |
| CN112566581B (en) | 2018-08-10 | 2024-03-19 | 柯惠有限合伙公司 | System for ablation visualization |
| WO2020081373A1 (en) | 2018-10-16 | 2020-04-23 | Bard Access Systems, Inc. | Safety-equipped connection systems and methods thereof for establishing electrical connections |
| US11553969B1 (en) | 2019-02-14 | 2023-01-17 | Onpoint Medical, Inc. | System for computation of object coordinates accounting for movement of a surgical site for spinal and other procedures |
| US11857378B1 (en) | 2019-02-14 | 2024-01-02 | Onpoint Medical, Inc. | Systems for adjusting and tracking head mounted displays during surgery including with surgical helmets |
| US20200281561A1 (en) | 2019-03-05 | 2020-09-10 | Ethos Medical, Inc. | Systems, Methods, and Devices for Instrument Guidance |
| US11571268B1 (en) * | 2019-04-02 | 2023-02-07 | Canon U.S.A., Inc. | Medical continuum robot extraction and methods thereof |
| US11154274B2 (en) | 2019-04-23 | 2021-10-26 | Decision Sciences Medical Company, LLC | Semi-rigid acoustic coupling articles for ultrasound diagnostic and treatment applications |
| US11446094B2 (en) | 2019-05-02 | 2022-09-20 | Medtronic Navigation, Inc. | Nasal patient tracking device and method of using the same |
| US11547491B2 (en) | 2019-05-02 | 2023-01-10 | Medtronic Navigation, Inc. | Oral patient tracking device and method of using the same |
| US11510692B2 (en) * | 2019-05-31 | 2022-11-29 | Biosense Webster (Israel) Ltd. | Ear-nose-throat (ENT) navigable shaver with ferromagnetic components |
| US11576729B2 (en) | 2019-06-17 | 2023-02-14 | Koninklijke Philips N.V. | Cranial surgery using optical shape sensing |
| KR102324002B1 (en) * | 2019-10-07 | 2021-11-08 | 대구가톨릭대학교산학협력단 | Device of coulomb-stimulated breaking up iron-oxide mineralization with protein aggregation using traversing ion beam and traversing ion beam dosimeter |
| US20210275255A1 (en) * | 2020-03-09 | 2021-09-09 | Biosense Webster (Israel) Ltd. | Finding roll angle of distal end of deflectable or non-deflectable invasive medical instrument |
| US11832883B2 (en) | 2020-04-23 | 2023-12-05 | Johnson & Johnson Surgical Vision, Inc. | Using real-time images for augmented-reality visualization of an ophthalmology surgical tool |
| US20210330394A1 (en) * | 2020-04-23 | 2021-10-28 | Johnson & Johnson Surgical Vision, Inc. | Augmented-reality visualization of an ophthalmic surgical tool |
| EP3903713A1 (en) | 2020-04-29 | 2021-11-03 | Stryker European Operations Limited | Field generator assembly and method for surgical navigation |
| US20240066322A1 (en) * | 2020-11-06 | 2024-02-29 | University Of Washington | Devices, systems, and methods for personalized dosimetry |
| WO2022099147A1 (en) | 2020-11-09 | 2022-05-12 | Bard Access Systems, Inc. | Medical device magnetizer |
| CN116685847A (en) | 2020-11-13 | 2023-09-01 | 决策科学医疗有限责任公司 | System and method for synthetic aperture ultrasound imaging of objects |
| US11786206B2 (en) | 2021-03-10 | 2023-10-17 | Onpoint Medical, Inc. | Augmented reality guidance for imaging systems |
Citations (92)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| US3644825A (en) * | 1969-12-31 | 1972-02-22 | Texas Instruments Inc | Magnetic detection system for detecting movement of an object utilizing signals derived from two orthogonal pickup coils |
| US3821469A (en) * | 1972-05-15 | 1974-06-28 | Amperex Electronic Corp | Graphical data device |
| US3868565A (en) * | 1973-07-30 | 1975-02-25 | Jack Kuipers | Object tracking and orientation determination means, system and process |
| US4017858A (en) * | 1973-07-30 | 1977-04-12 | Polhemus Navigation Sciences, Inc. | Apparatus for generating a nutating electromagnetic field |
| US4182312A (en) * | 1977-05-20 | 1980-01-08 | Mushabac David R | Dental probe |
| US4256112A (en) * | 1979-02-12 | 1981-03-17 | David Kopf Instruments | Head positioner |
| US4262306A (en) * | 1977-04-27 | 1981-04-14 | Karlheinz Renner | Method and apparatus for monitoring of positions of patients and/or radiation units |
| US4314251A (en) * | 1979-07-30 | 1982-02-02 | The Austin Company | Remote object position and orientation locater |
| US4319136A (en) * | 1979-11-09 | 1982-03-09 | Jinkins J Randolph | Computerized tomography radiograph data transfer cap |
| US4328548A (en) * | 1980-04-04 | 1982-05-04 | The Austin Company | Locator for source of electromagnetic radiation having unknown structure or orientation |
| US4341220A (en) * | 1979-04-13 | 1982-07-27 | Pfizer Inc. | Stereotactic surgery apparatus and method |
| US4506676A (en) * | 1982-09-10 | 1985-03-26 | Duska Alois A | Radiographic localization technique |
| US4583538A (en) * | 1984-05-04 | 1986-04-22 | Onik Gary M | Method and apparatus for stereotaxic placement of probes in the body utilizing CT scanner localization |
| US4638798A (en) * | 1980-09-10 | 1987-01-27 | Shelden C Hunter | Stereotactic method and apparatus for locating and treating or removing lesions |
| US4642786A (en) * | 1984-05-25 | 1987-02-10 | Position Orientation Systems, Ltd. | Method and apparatus for position and orientation measurement using a magnetic field and retransmission |
| US4651732A (en) * | 1983-03-17 | 1987-03-24 | Frederick Philip R | Three-dimensional light guidance system for invasive procedures |
| US4659971A (en) * | 1984-08-16 | 1987-04-21 | Seiko Instruments & Electronics Ltd. | Robot controlling system |
| US4660970A (en) * | 1983-11-25 | 1987-04-28 | Carl-Zeiss-Stiftung | Method and apparatus for the contact-less measuring of objects |
| US4722056A (en) * | 1986-02-18 | 1988-01-26 | Trustees Of Dartmouth College | Reference display systems for superimposing a tomagraphic image onto the focal plane of an operating microscope |
| US4723544A (en) * | 1986-07-09 | 1988-02-09 | Moore Robert R | Hemispherical vectoring needle guide for discolysis |
| US4733969A (en) * | 1986-09-08 | 1988-03-29 | Cyberoptics Corporation | Laser probe for determining distance |
| US4737032A (en) * | 1985-08-26 | 1988-04-12 | Cyberware Laboratory, Inc. | Surface mensuration sensor |
| US4737794A (en) * | 1985-12-09 | 1988-04-12 | Mcdonnell Douglas Corporation | Method and apparatus for determining remote object orientation and position |
| US4742356A (en) * | 1985-12-09 | 1988-05-03 | Mcdonnell Douglas Corporation | Method and apparatus for determining remote object orientation and position |
| US4743771A (en) * | 1985-06-17 | 1988-05-10 | View Engineering, Inc. | Z-axis height measurement system |
| US4742815A (en) * | 1986-01-02 | 1988-05-10 | Ninan Champil A | Computer monitoring of endoscope |
| US4743770A (en) * | 1986-09-22 | 1988-05-10 | Mitutoyo Mfg. Co., Ltd. | Profile-measuring light probe using a change in reflection factor in the proximity of a critical angle of light |
| US4745290A (en) * | 1987-03-19 | 1988-05-17 | David Frankel | Method and apparatus for use in making custom shoes |
| US4750487A (en) * | 1986-11-24 | 1988-06-14 | Zanetti Paul H | Stereotactic frame |
| US4753528A (en) * | 1983-12-13 | 1988-06-28 | Quantime, Inc. | Laser archery distance device |
| US4804261A (en) * | 1987-03-27 | 1989-02-14 | Kirschen David G | Anti-claustrophobic glasses |
| US4805615A (en) * | 1985-07-02 | 1989-02-21 | Carol Mark P | Method and apparatus for performing stereotactic surgery |
| US4809694A (en) * | 1987-05-19 | 1989-03-07 | Ferrara Vincent L | Biopsy guide |
| US4821200A (en) * | 1986-04-14 | 1989-04-11 | Jonkopings Lans Landsting | Method and apparatus for manufacturing a modified, three-dimensional reproduction of a soft, deformable object |
| US4821731A (en) * | 1986-04-25 | 1989-04-18 | Intra-Sonix, Inc. | Acoustic image system and method |
| US4822163A (en) * | 1986-06-26 | 1989-04-18 | Robotic Vision Systems, Inc. | Tracking vision sensor |
| US4825091A (en) * | 1987-02-05 | 1989-04-25 | Carl-Zeiss-Stiftung | Optoelectronic distance sensor with visible pilot beam |
| US4829373A (en) * | 1987-08-03 | 1989-05-09 | Vexcel Corporation | Stereo mensuration apparatus |
| US4836778A (en) * | 1987-05-26 | 1989-06-06 | Vexcel Corporation | Mandibular motion monitoring system |
| US4838265A (en) * | 1985-05-24 | 1989-06-13 | Cosman Eric R | Localization device for probe placement under CT scanner imaging |
| US4841967A (en) * | 1984-01-30 | 1989-06-27 | Chang Ming Z | Positioning device for percutaneous needle insertion |
| US4845305A (en) * | 1988-07-07 | 1989-07-04 | National Starch And Chemical Corporation | Process for the preparation of isophthaladehyde |
| US4923459A (en) * | 1987-09-14 | 1990-05-08 | Kabushiki Kaisha Toshiba | Stereotactics apparatus |
| US4931056A (en) * | 1987-09-04 | 1990-06-05 | Neurodynamics, Inc. | Catheter guide apparatus for perpendicular insertion into a cranium orifice |
| US4945305A (en) * | 1986-10-09 | 1990-07-31 | Ascension Technology Corporation | Device for quantitatively measuring the relative position and orientation of two bodies in the presence of metals utilizing direct current magnetic fields |
| US4991579A (en) * | 1987-11-10 | 1991-02-12 | Allen George S | Method and apparatus for providing related images over time of a portion of the anatomy using fiducial implants |
| US5017139A (en) * | 1990-07-05 | 1991-05-21 | Mushabac David R | Mechanical support for hand-held dental/medical instrument |
| US5027818A (en) * | 1987-12-03 | 1991-07-02 | University Of Florida | Dosimetric technique for stereotactic radiosurgery same |
| US5078140A (en) * | 1986-05-08 | 1992-01-07 | Kwoh Yik S | Imaging device - aided robotic stereotaxis system |
| US5086401A (en) * | 1990-05-11 | 1992-02-04 | International Business Machines Corporation | Image-directed robotic system for precise robotic surgery including redundant consistency checking |
| US5098426A (en) * | 1989-02-06 | 1992-03-24 | Phoenix Laser Systems, Inc. | Method and apparatus for precision laser surgery |
| US5099846A (en) * | 1988-12-23 | 1992-03-31 | Hardy Tyrone L | Method and apparatus for video presentation from a variety of scanner imaging sources |
| US5107839A (en) * | 1990-05-04 | 1992-04-28 | Pavel V. Houdek | Computer controlled stereotaxic radiotherapy system and method |
| US5186174A (en) * | 1987-05-21 | 1993-02-16 | G. M. Piaff | Process and device for the reproducible optical representation of a surgical operation |
| US5193106A (en) * | 1990-08-28 | 1993-03-09 | Desena Danforth | X-ray identification marker |
| US5197476A (en) * | 1989-03-16 | 1993-03-30 | Christopher Nowacki | Locating target in human body |
| US5207688A (en) * | 1991-10-31 | 1993-05-04 | Medco, Inc. | Noninvasive head fixation method and apparatus |
| US5211165A (en) * | 1991-09-03 | 1993-05-18 | General Electric Company | Tracking system to follow the position and orientation of a device with radiofrequency field gradients |
| US5224049A (en) * | 1990-04-10 | 1993-06-29 | Mushabac David R | Method, system and mold assembly for use in preparing a dental prosthesis |
| US5230338A (en) * | 1987-11-10 | 1993-07-27 | Allen George S | Interactive image-guided surgical system for displaying images corresponding to the placement of a surgical tool or the like |
| US5230623A (en) * | 1991-12-10 | 1993-07-27 | Radionics, Inc. | Operating pointer with interactive computergraphics |
| US5279309A (en) * | 1991-06-13 | 1994-01-18 | International Business Machines Corporation | Signaling device and method for monitoring positions in a surgical operation |
| US5285787A (en) * | 1989-09-12 | 1994-02-15 | Kabushiki Kaisha Toshiba | Apparatus for calculating coordinate data of desired point in subject to be examined |
| US5288253A (en) * | 1992-08-07 | 1994-02-22 | Nortrans Shipping And Trading Far East Pte Ltd. | Single point mooring system employing a submerged buoy and a vessel mounted fluid swivel |
| US5299253A (en) * | 1992-04-10 | 1994-03-29 | Akzo N.V. | Alignment system to overlay abdominal computer aided tomography and magnetic resonance anatomy with single photon emission tomography |
| US5300080A (en) * | 1991-11-01 | 1994-04-05 | David Clayman | Stereotactic instrument guided placement |
| US5306271A (en) * | 1992-03-09 | 1994-04-26 | Izi Corporation | Radiation therapy skin markers |
| US5307072A (en) * | 1992-07-09 | 1994-04-26 | Polhemus Incorporated | Non-concentricity compensation in position and orientation measurement systems |
| US5309913A (en) * | 1992-11-30 | 1994-05-10 | The Cleveland Clinic Foundation | Frameless stereotaxy system |
| US5330485A (en) * | 1991-11-01 | 1994-07-19 | Clayman David A | Cerebral instrument guide frame and procedures utilizing it |
| US5383454A (en) * | 1990-10-19 | 1995-01-24 | St. Louis University | System for indicating the position of a surgical probe within a head on an image of the head |
| US5389101A (en) * | 1992-04-21 | 1995-02-14 | University Of Utah | Apparatus and method for photogrammetric surgical localization |
| US5391199A (en) * | 1993-07-20 | 1995-02-21 | Biosense, Inc. | Apparatus and method for treating cardiac arrhythmias |
| US5394875A (en) * | 1993-10-21 | 1995-03-07 | Lewis; Judith T. | Automatic ultrasonic localization of targets implanted in a portion of the anatomy |
| US5480439A (en) * | 1991-02-13 | 1996-01-02 | Lunar Corporation | Method for periprosthetic bone mineral density measurement |
| US5483961A (en) * | 1993-03-19 | 1996-01-16 | Kelly; Patrick J. | Magnetic field digitizer for stereotactic surgery |
| US5517990A (en) * | 1992-11-30 | 1996-05-21 | The Cleveland Clinic Foundation | Stereotaxy wand and tool guide |
| US5600330A (en) * | 1994-07-12 | 1997-02-04 | Ascension Technology Corporation | Device for measuring position and orientation using non-dipole magnet IC fields |
| US5615132A (en) * | 1994-01-21 | 1997-03-25 | Crossbow Technology, Inc. | Method and apparatus for determining position and orientation of a moveable object using accelerometers |
| US5617857A (en) * | 1995-06-06 | 1997-04-08 | Image Guided Technologies, Inc. | Imaging system having interactive medical instruments and methods |
| US5622170A (en) * | 1990-10-19 | 1997-04-22 | Image Guided Technologies, Inc. | Apparatus for determining the position and orientation of an invasive portion of a probe inside a three-dimensional body |
| US5640170A (en) * | 1995-06-05 | 1997-06-17 | Polhemus Incorporated | Position and orientation measuring system having anti-distortion source configuration |
| US5718241A (en) * | 1995-06-07 | 1998-02-17 | Biosense, Inc. | Apparatus and method for treating cardiac arrhythmias with no discrete target |
| US5729129A (en) * | 1995-06-07 | 1998-03-17 | Biosense, Inc. | Magnetic location system with feedback adjustment of magnetic field generator |
| US5730130A (en) * | 1993-02-12 | 1998-03-24 | Johnson & Johnson Professional, Inc. | Localization cap for fiducial markers |
| US5738096A (en) * | 1993-07-20 | 1998-04-14 | Biosense, Inc. | Cardiac electromechanics |
| US5752513A (en) * | 1995-06-07 | 1998-05-19 | Biosense, Inc. | Method and apparatus for determining position of object |
| US5755725A (en) * | 1993-09-07 | 1998-05-26 | Deemed International, S.A. | Computer-assisted microsurgery methods and equipment |
| US5769861A (en) * | 1995-09-28 | 1998-06-23 | Brainlab Med. Computersysteme Gmbh | Method and devices for localizing an instrument |
| US5868675A (en) * | 1989-10-05 | 1999-02-09 | Elekta Igs S.A. | Interactive system for local intervention inside a nonhumogeneous structure |
| US5871445A (en) * | 1993-04-26 | 1999-02-16 | St. Louis University | System for indicating the position of a surgical probe within a head on an image of the head |
| US6071288A (en) * | 1994-09-30 | 2000-06-06 | Ohio Medical Instrument Company, Inc. | Apparatus and method for surgical stereotactic procedures |
Family Cites Families (224)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| US425112A (en) * | 1890-04-08 | John straiton | ||
| US581008A (en) * | 1897-04-20 | Bicycle-tire | ||
| DE482439C (en) | 1927-12-09 | 1929-09-14 | Fr Des Pompes Et Machines Wort | Feed water preheater for steam boilers of locomotives |
| US2650588A (en) | 1950-12-29 | 1953-09-01 | Drew Harry Guy Radcliffe | Artificial femoral head having an x-ray marker |
| US3109588A (en) * | 1962-01-26 | 1963-11-05 | William L Polhemus | Celestial computers |
| GB1257034A (en) * | 1968-03-25 | 1971-12-15 | ||
| US3991770A (en) * | 1974-01-24 | 1976-11-16 | Leveen Harry H | Method for treating benign and malignant tumors utilizing radio frequency, electromagnetic radiation |
| US3983474A (en) * | 1975-02-21 | 1976-09-28 | Polhemus Navigation Sciences, Inc. | Tracking and determining orientation of object using coordinate transformation means, system and process |
| US4054881A (en) * | 1976-04-26 | 1977-10-18 | The Austin Company | Remote object position locater |
| US4298874A (en) * | 1977-01-17 | 1981-11-03 | The Austin Company | Method and apparatus for tracking objects |
| DE2715106C2 (en) * | 1977-04-04 | 1982-05-27 | Siemens AG, 1000 Berlin und 8000 München | Device for measuring the location, the position and / or the change in location or position of a rigid body in space |
| US4173228A (en) | 1977-05-16 | 1979-11-06 | Applied Medical Devices | Catheter locating device |
| SU745505A1 (en) | 1977-09-28 | 1980-07-05 | Научно-Исследовательский Институт Экспериментальной Медицины Амн Ссср | Method of guiding stereotaxic tool on target point |
| US4202349A (en) | 1978-04-24 | 1980-05-13 | Jones James W | Radiopaque vessel markers |
| USRE32619E (en) * | 1978-11-20 | 1988-03-08 | Apparatus and method for nuclear magnetic resonance scanning and mapping | |
| US4608977A (en) * | 1979-08-29 | 1986-09-02 | Brown Russell A | System using computed tomography as for selective body treatment |
| US4419012A (en) | 1979-09-11 | 1983-12-06 | Elliott Brothers (London) Limited | Position measuring system |
| US4317078A (en) * | 1979-10-15 | 1982-02-23 | Ohio State University Research Foundation | Remote position and orientation detection employing magnetic flux linkage |
| US4346384A (en) * | 1980-06-30 | 1982-08-24 | The Austin Company | Remote object position and orientation locator |
| US4428748A (en) * | 1980-04-09 | 1984-01-31 | Peyman Gholam A | Combined ultrasonic emulsifier and mechanical cutter for surgery |
| US4688037A (en) * | 1980-08-18 | 1987-08-18 | Mcdonnell Douglas Corporation | Electromagnetic communications and switching system |
| US4339953A (en) | 1980-08-29 | 1982-07-20 | Aisin Seiki Company, Ltd. | Position sensor |
| AU7986682A (en) | 1981-02-12 | 1982-08-19 | New York University | Apparatus for stereotactic surgery |
| NL8101722A (en) * | 1981-04-08 | 1982-11-01 | Philips Nv | CONTOUR METER. |
| US4710708A (en) | 1981-04-27 | 1987-12-01 | Develco | Method and apparatus employing received independent magnetic field components of a transmitted alternating magnetic field for determining location |
| US4431005A (en) * | 1981-05-07 | 1984-02-14 | Mccormick Laboratories, Inc. | Method of and apparatus for determining very accurately the position of a device inside biological tissue |
| US4422041A (en) | 1981-07-30 | 1983-12-20 | The United States Of America As Represented By The Secretary Of The Army | Magnet position sensing system |
| US4396945A (en) | 1981-08-19 | 1983-08-02 | Solid Photography Inc. | Method of sensing the position and orientation of elements in space |
| US4961422A (en) | 1983-01-21 | 1990-10-09 | Marchosky J Alexander | Method and apparatus for volumetric interstitial conductive hyperthermia |
| NL8300965A (en) | 1983-03-17 | 1984-10-16 | Nicolaas Roelof Snijder | SYSTEM FOR EXAMINATION OF SKELETON PARTS OF THE BODY OF A LIVING ORIGIN, IN PARTICULAR THE SPIRIT OF THE HUMAN BODY. |
| US4613866A (en) * | 1983-05-13 | 1986-09-23 | Mcdonnell Douglas Corporation | Three dimensional digitizer with electromagnetic coupling |
| NL8302228A (en) * | 1983-06-22 | 1985-01-16 | Optische Ind De Oude Delft Nv | MEASURING SYSTEM FOR USING A TRIANGULAR PRINCIPLE, CONTACT-FREE MEASURING A DISTANCE GIVEN BY A SURFACE CONTOUR TO AN OBJECTIVE LEVEL. |
| US4618978A (en) * | 1983-10-21 | 1986-10-21 | Cosman Eric R | Means for localizing target coordinates in a body relative to a guidance system reference frame in any arbitrary plane as viewed by a tomographic image through the body |
| US4549555A (en) | 1984-02-17 | 1985-10-29 | Orthothronics Limited Partnership | Knee laxity evaluator and motion module/digitizer arrangement |
| US4571834A (en) * | 1984-02-17 | 1986-02-25 | Orthotronics Limited Partnership | Knee laxity evaluator and motion module/digitizer arrangement |
| US4649504A (en) * | 1984-05-22 | 1987-03-10 | Cae Electronics, Ltd. | Optical position and orientation measurement techniques |
| US4636798A (en) * | 1984-05-29 | 1987-01-13 | Seavey Engineering Associates, Inc. | Microwave lens for beam broadening with antenna feeds |
| US4617925A (en) * | 1984-10-01 | 1986-10-21 | Laitinen Lauri V | Adapter for definition of the position of brain structures |
| US4705395A (en) * | 1984-10-03 | 1987-11-10 | Diffracto Ltd. | Triangulation data integrity |
| US4706665A (en) * | 1984-12-17 | 1987-11-17 | Gouda Kasim I | Frame for stereotactic surgery |
| DE3500605A1 (en) | 1985-01-10 | 1986-07-10 | Markus Dr. 5300 Bonn Hansen | DEVICE FOR MEASURING THE POSITIONS AND MOVEMENTS OF THE LOWER JAW RELATIVE TO THE UPPER JAW |
| DE3508730A1 (en) * | 1985-03-12 | 1986-09-18 | Siemens AG, 1000 Berlin und 8000 München | Measuring device for medical purposes |
| US4782239A (en) * | 1985-04-05 | 1988-11-01 | Nippon Kogaku K. K. | Optical position measuring apparatus |
| SE447848B (en) * | 1985-06-14 | 1986-12-15 | Anders Bengtsson | INSTRUMENTS FOR SEATING SURFACE TOPOGRAPHY |
| JPS62327A (en) * | 1985-06-26 | 1987-01-06 | 間中 信也 | Apparatus for detecting position of operation region in head |
| US4705401A (en) * | 1985-08-12 | 1987-11-10 | Cyberware Laboratory Inc. | Rapid three-dimensional surface digitizer |
| IL76517A (en) * | 1985-09-27 | 1989-02-28 | Nessim Igal Levy | Distance measuring device |
| US4709156A (en) * | 1985-11-27 | 1987-11-24 | Ex-Cell-O Corporation | Method and apparatus for inspecting a surface |
| US4794262A (en) * | 1985-12-03 | 1988-12-27 | Yukio Sato | Method and apparatus for measuring profile of three-dimensional object |
| JP2685071B2 (en) | 1986-03-10 | 1997-12-03 | 三菱電機株式会社 | Numerical control unit |
| US4821220A (en) * | 1986-07-25 | 1989-04-11 | Tektronix, Inc. | System for animating program operation and displaying time-based relationships |
| US4791934A (en) * | 1986-08-07 | 1988-12-20 | Picker International, Inc. | Computer tomography assisted stereotactic surgery system and method |
| US4761072A (en) * | 1986-09-30 | 1988-08-02 | Diffracto Ltd. | Electro-optical sensors for manual control |
| US4849692A (en) | 1986-10-09 | 1989-07-18 | Ascension Technology Corporation | Device for quantitatively measuring the relative position and orientation of two bodies in the presence of metals utilizing direct current magnetic fields |
| US4875478A (en) * | 1987-04-10 | 1989-10-24 | Chen Harry H | Portable compression grid & needle holder |
| US4793355A (en) | 1987-04-17 | 1988-12-27 | Biomagnetic Technologies, Inc. | Apparatus for process for making biomagnetic measurements |
| JPH02503519A (en) * | 1987-05-27 | 1990-10-25 | サージカル ナビゲーション テクノロジース インコーポレーティッド(アン アフィリエイティッド カンパニー オブ ソファマー ダンネク グループ インコーポレーティッド) | Method and apparatus for reproducibly optically displaying surgical procedures |
| FR2618211B1 (en) * | 1987-07-15 | 1991-11-15 | Chardon Bernard | FRONTAL LIGHTING DEVICE FOR OBSERVING NARROW AND DEEP CAVITIES. |
| US4875165A (en) * | 1987-11-27 | 1989-10-17 | University Of Chicago | Method for determination of 3-D structure in biplane angiography |
| EP0326768A3 (en) | 1988-02-01 | 1991-01-23 | Faro Medical Technologies Inc. | Computer-aided surgery apparatus |
| US5251127A (en) * | 1988-02-01 | 1993-10-05 | Faro Medical Technologies Inc. | Computer-aided surgery apparatus |
| US4951653A (en) | 1988-03-02 | 1990-08-28 | Laboratory Equipment, Corp. | Ultrasound brain lesioning system |
| US4869247A (en) * | 1988-03-11 | 1989-09-26 | The University Of Virginia Alumni Patents Foundation | Video tumor fighting system |
| US4884566A (en) * | 1988-04-15 | 1989-12-05 | The University Of Michigan | System and method for determining orientation of planes of imaging |
| US5050608A (en) | 1988-07-12 | 1991-09-24 | Medirand, Inc. | System for indicating a position to be operated in a patient's body |
| US4896673A (en) * | 1988-07-15 | 1990-01-30 | Medstone International, Inc. | Method and apparatus for stone localization using ultrasound imaging |
| US4860331A (en) * | 1988-09-12 | 1989-08-22 | Williams John F | Image marker device |
| US4905698A (en) * | 1988-09-13 | 1990-03-06 | Pharmacia Deltec Inc. | Method and apparatus for catheter location determination |
| EP0359864B1 (en) | 1988-09-23 | 1993-12-01 | Siemens Aktiengesellschaft | Apparatus and method for the measurement of weak magnetic fields dependent upon position and time |
| US5265611A (en) | 1988-09-23 | 1993-11-30 | Siemens Aktiengellschaft | Apparatus for measuring weak, location-dependent and time-dependent magnetic field |
| US5143076A (en) | 1988-12-23 | 1992-09-01 | Tyrone L. Hardy | Three-dimensional beam localization microscope apparatus for stereotactic diagnoses or surgery |
| CN1049287A (en) * | 1989-05-24 | 1991-02-20 | 住友电气工业株式会社 | The treatment conduit |
| US5257998A (en) * | 1989-09-20 | 1993-11-02 | Mitaka Kohki Co., Ltd. | Medical three-dimensional locating apparatus |
| US5681260A (en) | 1989-09-22 | 1997-10-28 | Olympus Optical Co., Ltd. | Guiding apparatus for guiding an insertable body within an inspected object |
| EP0419729A1 (en) | 1989-09-29 | 1991-04-03 | Siemens Aktiengesellschaft | Position finding of a catheter by means of non-ionising fields |
| US5222499A (en) | 1989-11-15 | 1993-06-29 | Allen George S | Method and apparatus for imaging the anatomy |
| US5308352A (en) | 1989-11-17 | 1994-05-03 | Koutrouvelis Panos G | Stereotactic device |
| US5047036A (en) | 1989-11-17 | 1991-09-10 | Koutrouvelis Panos G | Stereotactic device |
| CA2260688A1 (en) | 1989-11-21 | 1991-05-21 | I.S.G. Technologies, Inc. | Probe-correlated viewing of anatomical image data |
| WO1991007913A1 (en) * | 1989-11-24 | 1991-06-13 | Technomed International | A method and apparatus for determining the position of a target relative to known co-ordinates |
| US5214615A (en) | 1990-02-26 | 1993-05-25 | Will Bauer | Three-dimensional displacement of a body with computer interface |
| US5253647A (en) | 1990-04-13 | 1993-10-19 | Olympus Optical Co., Ltd. | Insertion position and orientation state pickup for endoscope |
| US5295483A (en) * | 1990-05-11 | 1994-03-22 | Christopher Nowacki | Locating target in human body |
| US5457641A (en) | 1990-06-29 | 1995-10-10 | Sextant Avionique | Method and apparatus for determining an orientation associated with a mobile system, especially a line of sight inside a helmet visor |
| DE69112538T2 (en) | 1990-07-31 | 1996-03-21 | Faro Medical Technologies Inc | Computer aided surgical device. |
| GB9018660D0 (en) | 1990-08-24 | 1990-10-10 | Imperial College | Probe system |
| US5160337A (en) | 1990-09-24 | 1992-11-03 | Cosman Eric R | Curved-shaped floor stand for use with a linear accelerator in radiosurgery |
| US5198877A (en) * | 1990-10-15 | 1993-03-30 | Pixsys, Inc. | Method and apparatus for three-dimensional non-contact shape sensing |
| US5059789A (en) | 1990-10-22 | 1991-10-22 | International Business Machines Corp. | Optical position and orientation sensor |
| US5823958A (en) | 1990-11-26 | 1998-10-20 | Truppe; Michael | System and method for displaying a structural data image in real-time correlation with moveable body |
| US6006126A (en) | 1991-01-28 | 1999-12-21 | Cosman; Eric R. | System and method for stereotactic registration of image scan data |
| US5947981A (en) | 1995-01-31 | 1999-09-07 | Cosman; Eric R. | Head and neck localizer |
| US5662111A (en) | 1991-01-28 | 1997-09-02 | Cosman; Eric R. | Process of stereotactic optical navigation |
| US5339799A (en) | 1991-04-23 | 1994-08-23 | Olympus Optical Co., Ltd. | Medical system for reproducing a state of contact of the treatment section in the operation unit |
| US5291889A (en) * | 1991-05-23 | 1994-03-08 | Vanguard Imaging Ltd. | Apparatus and method for spatially positioning images |
| FI93607C (en) | 1991-05-24 | 1995-05-10 | John Koivukangas | Cutting Remedy |
| US5187475A (en) * | 1991-06-10 | 1993-02-16 | Honeywell Inc. | Apparatus for determining the position of an object |
| US5417210A (en) | 1992-05-27 | 1995-05-23 | International Business Machines Corporation | System and method for augmentation of endoscopic surgery |
| US5261404A (en) * | 1991-07-08 | 1993-11-16 | Mick Peter R | Three-dimensional mammal anatomy imaging system and method |
| US5249581A (en) | 1991-07-15 | 1993-10-05 | Horbal Mark T | Precision bone alignment |
| US5255680A (en) | 1991-09-03 | 1993-10-26 | General Electric Company | Automatic gantry positioning for imaging systems |
| EP0531081A1 (en) * | 1991-09-03 | 1993-03-10 | General Electric Company | Tracking system to follow the position and orientation of a device with radiofrequency fields |
| US5265610A (en) | 1991-09-03 | 1993-11-30 | General Electric Company | Multi-planar X-ray fluoroscopy system using radiofrequency fields |
| US5251635A (en) | 1991-09-03 | 1993-10-12 | General Electric Company | Stereoscopic X-ray fluoroscopy system using radiofrequency fields |
| US5645065A (en) | 1991-09-04 | 1997-07-08 | Navion Biomedical Corporation | Catheter depth, position and orientation location system |
| US5425367A (en) | 1991-09-04 | 1995-06-20 | Navion Biomedical Corporation | Catheter depth, position and orientation location system |
| DE4134481C2 (en) | 1991-10-18 | 1998-04-09 | Zeiss Carl Fa | Surgical microscope for computer-aided, stereotactic microsurgery |
| US5437277A (en) | 1991-11-18 | 1995-08-01 | General Electric Company | Inductively coupled RF tracking system for use in invasive imaging of a living body |
| US5445150A (en) | 1991-11-18 | 1995-08-29 | General Electric Company | Invasive system employing a radiofrequency tracking system |
| US5274551A (en) | 1991-11-29 | 1993-12-28 | General Electric Company | Method and apparatus for real-time navigation assist in interventional radiological procedures |
| US5371778A (en) | 1991-11-29 | 1994-12-06 | Picker International, Inc. | Concurrent display and adjustment of 3D projection, coronal slice, sagittal slice, and transverse slice images |
| DE4207632C2 (en) | 1992-03-11 | 1995-07-20 | Bodenseewerk Geraetetech | Device and method for positioning a body part for treatment purposes |
| DE4207901C3 (en) | 1992-03-12 | 1999-10-07 | Aesculap Ag & Co Kg | Method and device for displaying a work area in a three-dimensional structure |
| US5318025A (en) | 1992-04-01 | 1994-06-07 | General Electric Company | Tracking system to monitor the position and orientation of a device using multiplexed magnetic resonance detection |
| US5603318A (en) * | 1992-04-21 | 1997-02-18 | University Of Utah Research Foundation | Apparatus and method for photogrammetric surgical localization |
| IL102218A (en) | 1992-06-16 | 2003-06-24 | Elbit Systems Ltd | Tracker employing a rotating electromagnetic field |
| US5325873A (en) | 1992-07-23 | 1994-07-05 | Abbott Laboratories | Tube placement verifier system |
| DE4225112C1 (en) | 1992-07-30 | 1993-12-09 | Bodenseewerk Geraetetech | Instrument position relative to processing object measuring apparatus - has measuring device for measuring position of instrument including inertia sensor unit |
| FR2694881B1 (en) | 1992-07-31 | 1996-09-06 | Univ Joseph Fourier | METHOD FOR DETERMINING THE POSITION OF AN ORGAN. |
| EP0655138B1 (en) | 1992-08-14 | 1998-04-29 | BRITISH TELECOMMUNICATIONS public limited company | Position location system |
| CA2142338C (en) | 1992-08-14 | 1999-11-30 | John Stuart Bladen | Position location system |
| US5469847A (en) * | 1992-09-09 | 1995-11-28 | Izi Corporation | Radiographic multi-modality skin markers |
| US5368030A (en) * | 1992-09-09 | 1994-11-29 | Izi Corporation | Non-invasive multi-modality radiographic surface markers |
| US5647361A (en) | 1992-09-28 | 1997-07-15 | Fonar Corporation | Magnetic resonance imaging method and apparatus for guiding invasive therapy |
| DE4233978C1 (en) | 1992-10-08 | 1994-04-21 | Leibinger Gmbh | Body marking device for medical examinations |
| US5568384A (en) | 1992-10-13 | 1996-10-22 | Mayo Foundation For Medical Education And Research | Biomedical imaging and analysis |
| US5456718A (en) | 1992-11-17 | 1995-10-10 | Szymaitis; Dennis W. | Apparatus for detecting surgical objects within the human body |
| US5732703A (en) | 1992-11-30 | 1998-03-31 | The Cleveland Clinic Foundation | Stereotaxy wand and tool guide |
| US5353807A (en) | 1992-12-07 | 1994-10-11 | Demarco Thomas J | Magnetically guidable intubation device |
| US5353795A (en) | 1992-12-10 | 1994-10-11 | General Electric Company | Tracking system to monitor the position of a device using multiplexed magnetic resonance detection |
| US5575794A (en) * | 1993-02-12 | 1996-11-19 | Walus; Richard L. | Tool for implanting a fiducial marker |
| US5799099A (en) * | 1993-02-12 | 1998-08-25 | George S. Allen | Automatic technique for localizing externally attached fiducial markers in volume images of the head |
| US5787886A (en) | 1993-03-19 | 1998-08-04 | Compass International Incorporated | Magnetic field digitizer for stereotatic surgery |
| US5453686A (en) | 1993-04-08 | 1995-09-26 | Polhemus Incorporated | Pulsed-DC position and orientation measurement system |
| DE69424733T2 (en) | 1993-04-20 | 2001-02-01 | Gen Electric | GRAPHIC DIGITAL PROCESSING SYSTEM AND REAL-TIME VIDEO SYSTEM FOR IMPROVING THE REPRESENTATION OF BODY STRUCTURES DURING SURGICAL INTERVENTION. |
| US5387220A (en) * | 1993-06-15 | 1995-02-07 | Pisharodi; Maohaven | Stereotactic frame and localization method |
| US5425382A (en) | 1993-09-14 | 1995-06-20 | University Of Washington | Apparatus and method for locating a medical tube in the body of a patient |
| DE9314075U1 (en) * | 1993-09-17 | 1994-01-20 | Dwl Elektron Systeme Gmbh | Device for receiving at least one sonographic probe |
| US5558091A (en) | 1993-10-06 | 1996-09-24 | Biosense, Inc. | Magnetic determination of position and orientation |
| US5446548A (en) | 1993-10-08 | 1995-08-29 | Siemens Medical Systems, Inc. | Patient positioning and monitoring system |
| US5607436A (en) | 1993-10-08 | 1997-03-04 | United States Surgical Corporation | Apparatus for applying surgical clips |
| EP0649117A3 (en) | 1993-10-15 | 1996-01-31 | George S Allen | Method for providing medical images. |
| US5531227A (en) | 1994-01-28 | 1996-07-02 | Schneider Medical Technologies, Inc. | Imaging device and method |
| US6096048A (en) * | 1994-04-20 | 2000-08-01 | Howard, Iii; Matthew A. | Noninvasive, reattachable skull fiducial marker system |
| DE4417944A1 (en) | 1994-05-21 | 1995-11-23 | Zeiss Carl Fa | Process for correlating different coordinate systems in computer-assisted, stereotactic surgery |
| JP3267054B2 (en) | 1994-06-13 | 2002-03-18 | トヨタ自動車株式会社 | Power storage device for solar power |
| US5419325A (en) | 1994-06-23 | 1995-05-30 | General Electric Company | Magnetic resonance (MR) angiography using a faraday catheter |
| ATE188108T1 (en) | 1994-08-19 | 2000-01-15 | Biosense Inc | MEDICAL DIAGNOSIS, TREATMENT AND DISPLAY SYSTEM |
| US5999840A (en) * | 1994-09-01 | 1999-12-07 | Massachusetts Institute Of Technology | System and method of registration of three-dimensional data sets |
| US5531520A (en) | 1994-09-01 | 1996-07-02 | Massachusetts Institute Of Technology | System and method of registration of three-dimensional data sets including anatomical body data |
| US5829444A (en) * | 1994-09-15 | 1998-11-03 | Visualization Technology, Inc. | Position tracking and imaging system for use in medical applications |
| US5803089A (en) * | 1994-09-15 | 1998-09-08 | Visualization Technology, Inc. | Position tracking and imaging system for use in medical applications |
| US5611025A (en) * | 1994-11-23 | 1997-03-11 | General Electric Company | Virtual internal cavity inspection system |
| US5762064A (en) | 1995-01-23 | 1998-06-09 | Northrop Grumman Corporation | Medical magnetic positioning system and method for determining the position of a magnetic probe |
| US5682890A (en) | 1995-01-26 | 1997-11-04 | Picker International, Inc. | Magnetic resonance stereotactic surgery with exoskeleton tissue stabilization |
| US5971997A (en) | 1995-02-03 | 1999-10-26 | Radionics, Inc. | Intraoperative recalibration apparatus for stereotactic navigators |
| US5588430A (en) | 1995-02-14 | 1996-12-31 | University Of Florida Research Foundation, Inc. | Repeat fixation for frameless stereotactic procedure |
| US5797849A (en) | 1995-03-28 | 1998-08-25 | Sonometrics Corporation | Method for carrying out a medical procedure using a three-dimensional tracking and imaging system |
| US5730129A (en) * | 1995-04-03 | 1998-03-24 | General Electric Company | Imaging of interventional devices in a non-stationary subject |
| US5566681A (en) | 1995-05-02 | 1996-10-22 | Manwaring; Kim H. | Apparatus and method for stabilizing a body part |
| US6122541A (en) | 1995-05-04 | 2000-09-19 | Radionics, Inc. | Head band for frameless stereotactic registration |
| US5592939A (en) * | 1995-06-14 | 1997-01-14 | Martinelli; Michael A. | Method and system for navigating a catheter probe |
| US5638819A (en) | 1995-08-29 | 1997-06-17 | Manwaring; Kim H. | Method and apparatus for guiding an instrument to a target |
| US6351659B1 (en) * | 1995-09-28 | 2002-02-26 | Brainlab Med. Computersysteme Gmbh | Neuro-navigation system |
| US5715822A (en) * | 1995-09-28 | 1998-02-10 | General Electric Company | Magnetic resonance devices suitable for both tracking and imaging |
| US5772594A (en) | 1995-10-17 | 1998-06-30 | Barrick; Earl F. | Fluoroscopic image guided orthopaedic surgery system with intraoperative registration |
| US5697377A (en) | 1995-11-22 | 1997-12-16 | Medtronic, Inc. | Catheter mapping system and method |
| DE19547977A1 (en) * | 1995-12-21 | 1997-06-26 | Zeiss Carl Fa | Touch probe for coordinate measuring machines |
| US5682886A (en) | 1995-12-26 | 1997-11-04 | Musculographics Inc | Computer-assisted surgical system |
| US5727552A (en) * | 1996-01-11 | 1998-03-17 | Medtronic, Inc. | Catheter and electrical lead location system |
| US5711299A (en) * | 1996-01-26 | 1998-01-27 | Manwaring; Kim H. | Surgical guidance method and system for approaching a target within a body |
| US5769843A (en) | 1996-02-20 | 1998-06-23 | Cormedica | Percutaneous endomyocardial revascularization |
| US5828770A (en) | 1996-02-20 | 1998-10-27 | Northern Digital Inc. | System for determining the spatial position and angular orientation of an object |
| EP0886757B1 (en) | 1996-02-27 | 2005-05-25 | Biosense Webster, Inc. | Location system with field actuation sequences |
| US5727553A (en) * | 1996-03-25 | 1998-03-17 | Saad; Saad A. | Catheter with integral electromagnetic location identification device |
| US5782765A (en) | 1996-04-25 | 1998-07-21 | Medtronic, Inc. | Medical positioning system |
| US5799055A (en) | 1996-05-15 | 1998-08-25 | Northwestern University | Apparatus and method for planning a stereotactic surgical procedure using coordinated fluoroscopy |
| US6013087A (en) * | 1996-05-29 | 2000-01-11 | U.S. Philips Corporation | Image-guided surgery system |
| US5742394A (en) | 1996-06-14 | 1998-04-21 | Ascension Technology Corporation | Optical 6D measurement system with two fan shaped beams rotating around one axis |
| US5767669A (en) | 1996-06-14 | 1998-06-16 | Ascension Technology Corporation | Magnetic field position and orientation measurement system with dynamic eddy current rejection |
| US5767960A (en) | 1996-06-14 | 1998-06-16 | Ascension Technology Corporation | Optical 6D measurement system with three fan-shaped beams rotating around one axis |
| US5820553A (en) | 1996-08-16 | 1998-10-13 | Siemens Medical Systems, Inc. | Identification system and method for radiation therapy |
| US5744953A (en) | 1996-08-29 | 1998-04-28 | Ascension Technology Corporation | Magnetic motion tracker with transmitter placed on tracked object |
| US5831260A (en) | 1996-09-10 | 1998-11-03 | Ascension Technology Corporation | Hybrid motion tracker |
| US5951571A (en) | 1996-09-19 | 1999-09-14 | Surgical Navigation Specialist Inc. | Method and apparatus for correlating a body with an image of the body |
| US5980535A (en) | 1996-09-30 | 1999-11-09 | Picker International, Inc. | Apparatus for anatomical tracking |
| US6016439A (en) * | 1996-10-15 | 2000-01-18 | Biosense, Inc. | Method and apparatus for synthetic viewpoint imaging |
| US5810008A (en) | 1996-12-03 | 1998-09-22 | Isg Technologies Inc. | Apparatus and method for visualizing ultrasonic images |
| ES2208963T3 (en) * | 1997-01-03 | 2004-06-16 | Biosense, Inc. | PRESSURE SENSITIVE VASCULAR ENDOPROTESIS. |
| US5928248A (en) | 1997-02-14 | 1999-07-27 | Biosense, Inc. | Guided deployment of stents |
| US6006127A (en) | 1997-02-28 | 1999-12-21 | U.S. Philips Corporation | Image-guided surgery system |
| US6019725A (en) * | 1997-03-07 | 2000-02-01 | Sonometrics Corporation | Three-dimensional tracking and imaging system |
| DE19751761B4 (en) | 1997-04-11 | 2006-06-22 | Brainlab Ag | System and method for currently accurate detection of treatment targets |
| US5921992A (en) | 1997-04-11 | 1999-07-13 | Radionics, Inc. | Method and system for frameless tool calibration |
| DE19715202B4 (en) | 1997-04-11 | 2006-02-02 | Brainlab Ag | Referencing device with a mouthpiece |
| US5834759A (en) | 1997-05-22 | 1998-11-10 | Glossop; Neil David | Tracking device having emitter groups with different emitting directions |
| US5907395A (en) | 1997-06-06 | 1999-05-25 | Image Guided Technologies, Inc. | Optical fiber probe for position measurement |
| CA2240776C (en) | 1997-07-18 | 2006-01-10 | Image Guided Technologies, Inc. | Improved optical tracking system |
| US6096050A (en) | 1997-09-19 | 2000-08-01 | Surgical Navigation Specialist Inc. | Method and apparatus for correlating a body with an image of the body |
| US5987960A (en) | 1997-09-26 | 1999-11-23 | Picker International, Inc. | Tool calibrator |
| US5999837A (en) | 1997-09-26 | 1999-12-07 | Picker International, Inc. | Localizing and orienting probe for view devices |
| DE69738156T2 (en) | 1997-09-27 | 2008-06-12 | Brainlab Ag | Method and device for taking a three-dimensional image of a body part |
| US5978696A (en) | 1997-10-06 | 1999-11-02 | General Electric Company | Real-time image-guided placement of anchor devices |
| US6201387B1 (en) * | 1997-10-07 | 2001-03-13 | Biosense, Inc. | Miniaturized position sensor having photolithographic coils for tracking a medical probe |
| US6147480A (en) | 1997-10-23 | 2000-11-14 | Biosense, Inc. | Detection of metal disturbance |
| US5882304A (en) * | 1997-10-27 | 1999-03-16 | Picker Nordstar Corporation | Method and apparatus for determining probe location |
| DE19747427C2 (en) | 1997-10-28 | 1999-12-09 | Zeiss Carl Fa | Device for bone segment navigation |
| US6014580A (en) * | 1997-11-12 | 2000-01-11 | Stereotaxis, Inc. | Device and method for specifying magnetic field for surgical applications |
| US6149592A (en) | 1997-11-26 | 2000-11-21 | Picker International, Inc. | Integrated fluoroscopic projection image data, volumetric image data, and surgical device position data |
| US5938603A (en) | 1997-12-01 | 1999-08-17 | Cordis Webster, Inc. | Steerable catheter with electromagnetic sensor |
| US5967982A (en) | 1997-12-09 | 1999-10-19 | The Cleveland Clinic Foundation | Non-invasive spine and bone registration for frameless stereotaxy |
| ES2253882T3 (en) | 1998-03-30 | 2006-06-01 | Biosense Webster, Inc. | THREE AXLE COIL SENSOR. |
| DE19829224B4 (en) | 1998-06-30 | 2005-12-15 | Brainlab Ag | Method for localizing treatment goals in the area of soft body parts |
| US6148229A (en) * | 1998-12-07 | 2000-11-14 | Medrad, Inc. | System and method for compensating for motion artifacts in a strong magnetic field |
| US6285902B1 (en) | 1999-02-10 | 2001-09-04 | Surgical Insights, Inc. | Computer assisted targeting device for use in orthopaedic surgery |
| DE19917867B4 (en) * | 1999-04-20 | 2005-04-21 | Brainlab Ag | Method and device for image support in the treatment of treatment objectives with integration of X-ray detection and navigation system |
| US6381485B1 (en) * | 1999-10-28 | 2002-04-30 | Surgical Navigation Technologies, Inc. | Registration of human anatomy integrated for electromagnetic localization |
| DE19953177A1 (en) * | 1999-11-04 | 2001-06-21 | Brainlab Ag | Method to position patient exactly for radiation therapy or surgery; involves comparing positions in landmarks in X-ray image and reconstructed image date, to determine positioning errors |
| DE19956814B4 (en) | 1999-11-25 | 2004-07-15 | Brainlab Ag | Shape detection of treatment devices |
| US7747312B2 (en) * | 2000-01-04 | 2010-06-29 | George Mason Intellectual Properties, Inc. | System and method for automatic shape registration and instrument tracking |
| DE10000937B4 (en) | 2000-01-12 | 2006-02-23 | Brainlab Ag | Intraoperative navigation update |
| US6484049B1 (en) | 2000-04-28 | 2002-11-19 | Ge Medical Systems Global Technology Company, Llc | Fluoroscopic tracking and visualization system |
| US6478802B2 (en) | 2000-06-09 | 2002-11-12 | Ge Medical Systems Global Technology Company, Llc | Method and apparatus for display of an image guided drill bit |
| EP1190676B1 (en) | 2000-09-26 | 2003-08-13 | BrainLAB AG | Device for determining the position of a cutting guide |
-
1995
- 1995-09-13 US US08/527,517 patent/US5803089A/en not_active Expired - Lifetime
- 1995-09-13 EP EP99114366A patent/EP0951874A3/en not_active Ceased
- 1995-09-13 AT AT95932502T patent/ATE252349T1/en active
- 1995-09-13 DE DE69531994T patent/DE69531994T2/en not_active Expired - Lifetime
-
1996
- 1996-04-24 US US08/638,945 patent/US5676673A/en not_active Expired - Lifetime
- 1996-04-24 US US08/637,131 patent/US5800352A/en not_active Expired - Lifetime
- 1996-04-24 US US08/637,289 patent/US5873822A/en not_active Expired - Lifetime
-
1998
- 1998-12-15 US US09/212,024 patent/US6175756B1/en not_active Expired - Lifetime
-
1999
- 1999-03-25 JP JP08263199A patent/JP3325533B2/en not_active Expired - Lifetime
-
2000
- 2000-08-22 US US09/643,608 patent/US6694167B1/en not_active Expired - Lifetime
- 2000-08-22 US US09/643,815 patent/US6738656B1/en not_active Expired - Fee Related
- 2000-08-22 US US09/643,271 patent/US6687531B1/en not_active Expired - Lifetime
- 2000-10-11 US US09/686,188 patent/US6341231B1/en not_active Expired - Fee Related
-
2003
- 2003-04-30 US US10/427,472 patent/US20040024309A1/en not_active Abandoned
-
2005
- 2005-08-19 US US11/207,306 patent/US20060036151A1/en not_active Abandoned
-
2006
- 2006-11-21 US US11/602,640 patent/US8473026B2/en not_active Expired - Fee Related
Patent Citations (100)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| US3644825A (en) * | 1969-12-31 | 1972-02-22 | Texas Instruments Inc | Magnetic detection system for detecting movement of an object utilizing signals derived from two orthogonal pickup coils |
| US3821469A (en) * | 1972-05-15 | 1974-06-28 | Amperex Electronic Corp | Graphical data device |
| US3868565A (en) * | 1973-07-30 | 1975-02-25 | Jack Kuipers | Object tracking and orientation determination means, system and process |
| US4017858A (en) * | 1973-07-30 | 1977-04-12 | Polhemus Navigation Sciences, Inc. | Apparatus for generating a nutating electromagnetic field |
| US4262306A (en) * | 1977-04-27 | 1981-04-14 | Karlheinz Renner | Method and apparatus for monitoring of positions of patients and/or radiation units |
| US4182312A (en) * | 1977-05-20 | 1980-01-08 | Mushabac David R | Dental probe |
| US4256112A (en) * | 1979-02-12 | 1981-03-17 | David Kopf Instruments | Head positioner |
| US4341220A (en) * | 1979-04-13 | 1982-07-27 | Pfizer Inc. | Stereotactic surgery apparatus and method |
| US4314251A (en) * | 1979-07-30 | 1982-02-02 | The Austin Company | Remote object position and orientation locater |
| US4319136A (en) * | 1979-11-09 | 1982-03-09 | Jinkins J Randolph | Computerized tomography radiograph data transfer cap |
| US4328548A (en) * | 1980-04-04 | 1982-05-04 | The Austin Company | Locator for source of electromagnetic radiation having unknown structure or orientation |
| US4638798A (en) * | 1980-09-10 | 1987-01-27 | Shelden C Hunter | Stereotactic method and apparatus for locating and treating or removing lesions |
| US4506676A (en) * | 1982-09-10 | 1985-03-26 | Duska Alois A | Radiographic localization technique |
| US4651732A (en) * | 1983-03-17 | 1987-03-24 | Frederick Philip R | Three-dimensional light guidance system for invasive procedures |
| US4660970A (en) * | 1983-11-25 | 1987-04-28 | Carl-Zeiss-Stiftung | Method and apparatus for the contact-less measuring of objects |
| US4753528A (en) * | 1983-12-13 | 1988-06-28 | Quantime, Inc. | Laser archery distance device |
| US4841967A (en) * | 1984-01-30 | 1989-06-27 | Chang Ming Z | Positioning device for percutaneous needle insertion |
| US4583538A (en) * | 1984-05-04 | 1986-04-22 | Onik Gary M | Method and apparatus for stereotaxic placement of probes in the body utilizing CT scanner localization |
| US4642786A (en) * | 1984-05-25 | 1987-02-10 | Position Orientation Systems, Ltd. | Method and apparatus for position and orientation measurement using a magnetic field and retransmission |
| US4659971A (en) * | 1984-08-16 | 1987-04-21 | Seiko Instruments & Electronics Ltd. | Robot controlling system |
| US4838265A (en) * | 1985-05-24 | 1989-06-13 | Cosman Eric R | Localization device for probe placement under CT scanner imaging |
| US4743771A (en) * | 1985-06-17 | 1988-05-10 | View Engineering, Inc. | Z-axis height measurement system |
| US4805615A (en) * | 1985-07-02 | 1989-02-21 | Carol Mark P | Method and apparatus for performing stereotactic surgery |
| US4737032A (en) * | 1985-08-26 | 1988-04-12 | Cyberware Laboratory, Inc. | Surface mensuration sensor |
| US4737794A (en) * | 1985-12-09 | 1988-04-12 | Mcdonnell Douglas Corporation | Method and apparatus for determining remote object orientation and position |
| US4742356A (en) * | 1985-12-09 | 1988-05-03 | Mcdonnell Douglas Corporation | Method and apparatus for determining remote object orientation and position |
| US4742815A (en) * | 1986-01-02 | 1988-05-10 | Ninan Champil A | Computer monitoring of endoscope |
| US4722056A (en) * | 1986-02-18 | 1988-01-26 | Trustees Of Dartmouth College | Reference display systems for superimposing a tomagraphic image onto the focal plane of an operating microscope |
| US4821200A (en) * | 1986-04-14 | 1989-04-11 | Jonkopings Lans Landsting | Method and apparatus for manufacturing a modified, three-dimensional reproduction of a soft, deformable object |
| US4821731A (en) * | 1986-04-25 | 1989-04-18 | Intra-Sonix, Inc. | Acoustic image system and method |
| US5078140A (en) * | 1986-05-08 | 1992-01-07 | Kwoh Yik S | Imaging device - aided robotic stereotaxis system |
| US4822163A (en) * | 1986-06-26 | 1989-04-18 | Robotic Vision Systems, Inc. | Tracking vision sensor |
| US4723544A (en) * | 1986-07-09 | 1988-02-09 | Moore Robert R | Hemispherical vectoring needle guide for discolysis |
| US4733969A (en) * | 1986-09-08 | 1988-03-29 | Cyberoptics Corporation | Laser probe for determining distance |
| US4743770A (en) * | 1986-09-22 | 1988-05-10 | Mitutoyo Mfg. Co., Ltd. | Profile-measuring light probe using a change in reflection factor in the proximity of a critical angle of light |
| US4945305A (en) * | 1986-10-09 | 1990-07-31 | Ascension Technology Corporation | Device for quantitatively measuring the relative position and orientation of two bodies in the presence of metals utilizing direct current magnetic fields |
| US4750487A (en) * | 1986-11-24 | 1988-06-14 | Zanetti Paul H | Stereotactic frame |
| US4825091A (en) * | 1987-02-05 | 1989-04-25 | Carl-Zeiss-Stiftung | Optoelectronic distance sensor with visible pilot beam |
| US4745290A (en) * | 1987-03-19 | 1988-05-17 | David Frankel | Method and apparatus for use in making custom shoes |
| US4804261A (en) * | 1987-03-27 | 1989-02-14 | Kirschen David G | Anti-claustrophobic glasses |
| US4809694A (en) * | 1987-05-19 | 1989-03-07 | Ferrara Vincent L | Biopsy guide |
| US5186174A (en) * | 1987-05-21 | 1993-02-16 | G. M. Piaff | Process and device for the reproducible optical representation of a surgical operation |
| US4836778A (en) * | 1987-05-26 | 1989-06-06 | Vexcel Corporation | Mandibular motion monitoring system |
| US4829373A (en) * | 1987-08-03 | 1989-05-09 | Vexcel Corporation | Stereo mensuration apparatus |
| US4931056A (en) * | 1987-09-04 | 1990-06-05 | Neurodynamics, Inc. | Catheter guide apparatus for perpendicular insertion into a cranium orifice |
| US4923459A (en) * | 1987-09-14 | 1990-05-08 | Kabushiki Kaisha Toshiba | Stereotactics apparatus |
| US5094241A (en) * | 1987-11-10 | 1992-03-10 | Allen George S | Apparatus for imaging the anatomy |
| US5119817A (en) * | 1987-11-10 | 1992-06-09 | Allen George S | Apparatus for imaging the anatomy |
| US5230338A (en) * | 1987-11-10 | 1993-07-27 | Allen George S | Interactive image-guided surgical system for displaying images corresponding to the placement of a surgical tool or the like |
| US5016639A (en) * | 1987-11-10 | 1991-05-21 | Allen George S | Method and apparatus for imaging the anatomy |
| US5178164A (en) * | 1987-11-10 | 1993-01-12 | Allen George S | Method for implanting a fiducial implant into a patient |
| US4991579A (en) * | 1987-11-10 | 1991-02-12 | Allen George S | Method and apparatus for providing related images over time of a portion of the anatomy using fiducial implants |
| US5211164A (en) * | 1987-11-10 | 1993-05-18 | Allen George S | Method of locating a target on a portion of anatomy |
| US5097839A (en) * | 1987-11-10 | 1992-03-24 | Allen George S | Apparatus for imaging the anatomy |
| US5027818A (en) * | 1987-12-03 | 1991-07-02 | University Of Florida | Dosimetric technique for stereotactic radiosurgery same |
| US4845305A (en) * | 1988-07-07 | 1989-07-04 | National Starch And Chemical Corporation | Process for the preparation of isophthaladehyde |
| US5099846A (en) * | 1988-12-23 | 1992-03-31 | Hardy Tyrone L | Method and apparatus for video presentation from a variety of scanner imaging sources |
| US5098426A (en) * | 1989-02-06 | 1992-03-24 | Phoenix Laser Systems, Inc. | Method and apparatus for precision laser surgery |
| US5197476A (en) * | 1989-03-16 | 1993-03-30 | Christopher Nowacki | Locating target in human body |
| US5285787A (en) * | 1989-09-12 | 1994-02-15 | Kabushiki Kaisha Toshiba | Apparatus for calculating coordinate data of desired point in subject to be examined |
| US5868675A (en) * | 1989-10-05 | 1999-02-09 | Elekta Igs S.A. | Interactive system for local intervention inside a nonhumogeneous structure |
| US5224049A (en) * | 1990-04-10 | 1993-06-29 | Mushabac David R | Method, system and mold assembly for use in preparing a dental prosthesis |
| US5107839A (en) * | 1990-05-04 | 1992-04-28 | Pavel V. Houdek | Computer controlled stereotaxic radiotherapy system and method |
| US5086401A (en) * | 1990-05-11 | 1992-02-04 | International Business Machines Corporation | Image-directed robotic system for precise robotic surgery including redundant consistency checking |
| US5017139A (en) * | 1990-07-05 | 1991-05-21 | Mushabac David R | Mechanical support for hand-held dental/medical instrument |
| US5193106A (en) * | 1990-08-28 | 1993-03-09 | Desena Danforth | X-ray identification marker |
| US5383454B1 (en) * | 1990-10-19 | 1996-12-31 | Univ St Louis | System for indicating the position of a surgical probe within a head on an image of the head |
| US5891034A (en) * | 1990-10-19 | 1999-04-06 | St. Louis University | System for indicating the position of a surgical probe within a head on an image of the head |
| US5622170A (en) * | 1990-10-19 | 1997-04-22 | Image Guided Technologies, Inc. | Apparatus for determining the position and orientation of an invasive portion of a probe inside a three-dimensional body |
| US5383454A (en) * | 1990-10-19 | 1995-01-24 | St. Louis University | System for indicating the position of a surgical probe within a head on an image of the head |
| US5480439A (en) * | 1991-02-13 | 1996-01-02 | Lunar Corporation | Method for periprosthetic bone mineral density measurement |
| US5279309A (en) * | 1991-06-13 | 1994-01-18 | International Business Machines Corporation | Signaling device and method for monitoring positions in a surgical operation |
| US5211165A (en) * | 1991-09-03 | 1993-05-18 | General Electric Company | Tracking system to follow the position and orientation of a device with radiofrequency field gradients |
| US5207688A (en) * | 1991-10-31 | 1993-05-04 | Medco, Inc. | Noninvasive head fixation method and apparatus |
| US5300080A (en) * | 1991-11-01 | 1994-04-05 | David Clayman | Stereotactic instrument guided placement |
| US5330485A (en) * | 1991-11-01 | 1994-07-19 | Clayman David A | Cerebral instrument guide frame and procedures utilizing it |
| US5230623A (en) * | 1991-12-10 | 1993-07-27 | Radionics, Inc. | Operating pointer with interactive computergraphics |
| US5306271A (en) * | 1992-03-09 | 1994-04-26 | Izi Corporation | Radiation therapy skin markers |
| US5299253A (en) * | 1992-04-10 | 1994-03-29 | Akzo N.V. | Alignment system to overlay abdominal computer aided tomography and magnetic resonance anatomy with single photon emission tomography |
| US5389101A (en) * | 1992-04-21 | 1995-02-14 | University Of Utah | Apparatus and method for photogrammetric surgical localization |
| US5307072A (en) * | 1992-07-09 | 1994-04-26 | Polhemus Incorporated | Non-concentricity compensation in position and orientation measurement systems |
| US5288253A (en) * | 1992-08-07 | 1994-02-22 | Nortrans Shipping And Trading Far East Pte Ltd. | Single point mooring system employing a submerged buoy and a vessel mounted fluid swivel |
| US5517990A (en) * | 1992-11-30 | 1996-05-21 | The Cleveland Clinic Foundation | Stereotaxy wand and tool guide |
| US5309913A (en) * | 1992-11-30 | 1994-05-10 | The Cleveland Clinic Foundation | Frameless stereotaxy system |
| US5730130A (en) * | 1993-02-12 | 1998-03-24 | Johnson & Johnson Professional, Inc. | Localization cap for fiducial markers |
| US5483961A (en) * | 1993-03-19 | 1996-01-16 | Kelly; Patrick J. | Magnetic field digitizer for stereotactic surgery |
| US5871445A (en) * | 1993-04-26 | 1999-02-16 | St. Louis University | System for indicating the position of a surgical probe within a head on an image of the head |
| US5738096A (en) * | 1993-07-20 | 1998-04-14 | Biosense, Inc. | Cardiac electromechanics |
| US5391199A (en) * | 1993-07-20 | 1995-02-21 | Biosense, Inc. | Apparatus and method for treating cardiac arrhythmias |
| US5755725A (en) * | 1993-09-07 | 1998-05-26 | Deemed International, S.A. | Computer-assisted microsurgery methods and equipment |
| US5394875A (en) * | 1993-10-21 | 1995-03-07 | Lewis; Judith T. | Automatic ultrasonic localization of targets implanted in a portion of the anatomy |
| US5615132A (en) * | 1994-01-21 | 1997-03-25 | Crossbow Technology, Inc. | Method and apparatus for determining position and orientation of a moveable object using accelerometers |
| US5600330A (en) * | 1994-07-12 | 1997-02-04 | Ascension Technology Corporation | Device for measuring position and orientation using non-dipole magnet IC fields |
| US6071288A (en) * | 1994-09-30 | 2000-06-06 | Ohio Medical Instrument Company, Inc. | Apparatus and method for surgical stereotactic procedures |
| US5640170A (en) * | 1995-06-05 | 1997-06-17 | Polhemus Incorporated | Position and orientation measuring system having anti-distortion source configuration |
| US5617857A (en) * | 1995-06-06 | 1997-04-08 | Image Guided Technologies, Inc. | Imaging system having interactive medical instruments and methods |
| US5718241A (en) * | 1995-06-07 | 1998-02-17 | Biosense, Inc. | Apparatus and method for treating cardiac arrhythmias with no discrete target |
| US5752513A (en) * | 1995-06-07 | 1998-05-19 | Biosense, Inc. | Method and apparatus for determining position of object |
| US5729129A (en) * | 1995-06-07 | 1998-03-17 | Biosense, Inc. | Magnetic location system with feedback adjustment of magnetic field generator |
| US5769861A (en) * | 1995-09-28 | 1998-06-23 | Brainlab Med. Computersysteme Gmbh | Method and devices for localizing an instrument |
Cited By (243)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| USRE43952E1 (en) | 1989-10-05 | 2013-01-29 | Medtronic Navigation, Inc. | Interactive system for local intervention inside a non-homogeneous structure |
| US20070167722A1 (en) * | 1992-08-14 | 2007-07-19 | British Telecommunications Public Limited Company | Surgical navigation |
| US8200314B2 (en) | 1992-08-14 | 2012-06-12 | British Telecommunications Public Limited Company | Surgical navigation |
| US6832985B2 (en) * | 1997-04-16 | 2004-12-21 | Karl Storz Gmbh & Co. Kg | Endoscopic system with instrument position and orientation display |
| US20020188172A1 (en) * | 1997-04-16 | 2002-12-12 | Klaus Irion | Endoscopic system |
| USRE42194E1 (en) | 1997-09-24 | 2011-03-01 | Medtronic Navigation, Inc. | Percutaneous registration apparatus and method for use in computer-assisted surgical navigation |
| USRE42226E1 (en) | 1997-09-24 | 2011-03-15 | Medtronic Navigation, Inc. | Percutaneous registration apparatus and method for use in computer-assisted surgical navigation |
| USRE44305E1 (en) | 1997-09-24 | 2013-06-18 | Medtronic Navigation, Inc. | Percutaneous registration apparatus and method for use in computer-assisted surgical navigation |
| USRE46422E1 (en) | 1997-11-20 | 2017-06-06 | Medtronic Navigation, Inc. | Image guided awl/tap/screwdriver |
| USRE43328E1 (en) | 1997-11-20 | 2012-04-24 | Medtronic Navigation, Inc | Image guided awl/tap/screwdriver |
| USRE46409E1 (en) | 1997-11-20 | 2017-05-23 | Medtronic Navigation, Inc. | Image guided awl/tap/screwdriver |
| US8105339B2 (en) | 1997-12-12 | 2012-01-31 | Sofamor Danek Holdings, Inc. | Image guided spinal surgery guide system and method for use thereof |
| US7763035B2 (en) | 1997-12-12 | 2010-07-27 | Medtronic Navigation, Inc. | Image guided spinal surgery guide, system and method for use thereof |
| US20100286713A1 (en) * | 1997-12-12 | 2010-11-11 | Medtronic Navigation, Inc. | Image Guided Spinal Surgery Guide System And Method For Use Thereof |
| US20050059885A1 (en) * | 1997-12-12 | 2005-03-17 | Tony Melkent | Image guided spinal surgery guide, system and method for use thereof |
| US8768437B2 (en) | 1998-08-20 | 2014-07-01 | Sofamor Danek Holdings, Inc. | Fluoroscopic image guided surgery system with intraoperative registration |
| US7996064B2 (en) | 1999-03-23 | 2011-08-09 | Medtronic Navigation, Inc. | System and method for placing and determining an appropriately sized surgical implant |
| US20100041985A1 (en) * | 1999-03-23 | 2010-02-18 | Surgical Navigation Technologies, Inc. | Navigational Guidance Via Computer-Assisted Fluoroscopic Imaging |
| US20030073901A1 (en) * | 1999-03-23 | 2003-04-17 | Simon David A. | Navigational guidance via computer-assisted fluoroscopic imaging |
| US8845655B2 (en) | 1999-04-20 | 2014-09-30 | Medtronic Navigation, Inc. | Instrument guide system |
| US20100305580A1 (en) * | 1999-04-20 | 2010-12-02 | Medtronic Navigation, Inc | Instrument Guide System |
| US20030114752A1 (en) * | 1999-04-20 | 2003-06-19 | Jaimie Henderson | Instrument guidance method and system for image guided surgery |
| US9504530B2 (en) | 1999-10-28 | 2016-11-29 | Medtronic Navigation, Inc. | Method and apparatus for surgical navigation |
| US7657300B2 (en) | 1999-10-28 | 2010-02-02 | Medtronic Navigation, Inc. | Registration of human anatomy integrated for electromagnetic localization |
| US11331150B2 (en) | 1999-10-28 | 2022-05-17 | Medtronic Navigation, Inc. | Method and apparatus for surgical navigation |
| US20100137707A1 (en) * | 1999-10-28 | 2010-06-03 | Medtronic Navigation, Inc | Registration of Human Anatomy Integrated for Electromagnetic Localization |
| US20100331671A1 (en) * | 1999-10-28 | 2010-12-30 | Medtronic Navigation, Inc | Method and System for Navigating a Catheter Probe in the Presence of Field-Influencing Objects |
| US20020156363A1 (en) * | 1999-10-28 | 2002-10-24 | Hunter Mark W. | Registration of human anatomy integrated for electromagnetic localization |
| US8548565B2 (en) | 1999-10-28 | 2013-10-01 | Medtronic Navigation, Inc. | Registration of human anatomy integrated for electromagnetic localization |
| US8057407B2 (en) | 1999-10-28 | 2011-11-15 | Medtronic Navigation, Inc. | Surgical sensor |
| US20060278247A1 (en) * | 1999-10-28 | 2006-12-14 | Mark W. Hunter Et Al. | Surgical communication and power system |
| US8644907B2 (en) | 1999-10-28 | 2014-02-04 | Medtronic Navigaton, Inc. | Method and apparatus for surgical navigation |
| US8074662B2 (en) | 1999-10-28 | 2011-12-13 | Medtronic Navigation, Inc. | Surgical communication and power system |
| US7797032B2 (en) | 1999-10-28 | 2010-09-14 | Medtronic Navigation, Inc. | Method and system for navigating a catheter probe in the presence of field-influencing objects |
| US8290572B2 (en) | 1999-10-28 | 2012-10-16 | Medtronic Navigation, Inc. | Method and system for navigating a catheter probe in the presence of field-influencing objects |
| US20100210939A1 (en) * | 1999-10-28 | 2010-08-19 | Medtronic Navigation, Inc. | Method and Apparatus for Surgical Navigation |
| US20030117135A1 (en) * | 1999-10-28 | 2003-06-26 | Martinelli Michael A. | Method and system for navigating a catheter probe in the presence of field-influencing objects |
| US7881770B2 (en) | 2000-03-01 | 2011-02-01 | Medtronic Navigation, Inc. | Multiple cannula image guided tool for image guided procedures |
| US10898153B2 (en) | 2000-03-01 | 2021-01-26 | Medtronic Navigation, Inc. | Multiple cannula image guided tool for image guided procedures |
| US20110118593A1 (en) * | 2000-03-01 | 2011-05-19 | Medtronic Navigation, Inc. | Multiple Cannula Image Guided Tool for Image Guided Procedures |
| US20050113809A1 (en) * | 2000-03-01 | 2005-05-26 | Melkent Anthony J. | Multiple cannula image guided tool for image guided procedures |
| US8634897B2 (en) | 2000-04-07 | 2014-01-21 | Medtronic Navigation, Inc. | Trajectory storage apparatus and method for surgical navigation systems |
| US7853305B2 (en) | 2000-04-07 | 2010-12-14 | Medtronic Navigation, Inc. | Trajectory storage apparatus and method for surgical navigation systems |
| US20110077508A1 (en) * | 2000-04-07 | 2011-03-31 | Medtronic Navigation, Inc | Trajectory Storage Apparatus And Method For Surgical Navigation Systems |
| US20110052008A1 (en) * | 2000-06-14 | 2011-03-03 | Medtronic Navigation, Inc. | System and Method for Image Based Sensor Calibration |
| US20060262961A1 (en) * | 2000-06-14 | 2006-11-23 | Troy Holsing Et Al. | System and method for image based sensor calibration |
| US8320653B2 (en) | 2000-06-14 | 2012-11-27 | Medtronic Navigation, Inc. | System and method for image based sensor calibration |
| US7831082B2 (en) | 2000-06-14 | 2010-11-09 | Medtronic Navigation, Inc. | System and method for image based sensor calibration |
| US20040087852A1 (en) * | 2001-02-06 | 2004-05-06 | Edward Chen | Computer-assisted surgical positioning method and system |
| US20040181149A1 (en) * | 2001-02-07 | 2004-09-16 | Ulrich Langlotz | Device and method for intraoperative navigation |
| US20090287443A1 (en) * | 2001-06-04 | 2009-11-19 | Surgical Navigation Technologies, Inc. | Method for Calibrating a Navigation System |
| US9675424B2 (en) | 2001-06-04 | 2017-06-13 | Surgical Navigation Technologies, Inc. | Method for calibrating a navigation system |
| US20050273004A1 (en) * | 2002-02-28 | 2005-12-08 | Simon David A | Method and apparatus for perspective inversion |
| US20090262111A1 (en) * | 2002-02-28 | 2009-10-22 | Surgical Navigation Technologies, Inc. | Method and Apparatus for Perspective Inversion |
| US9757087B2 (en) | 2002-02-28 | 2017-09-12 | Medtronic Navigation, Inc. | Method and apparatus for perspective inversion |
| US8838199B2 (en) | 2002-04-04 | 2014-09-16 | Medtronic Navigation, Inc. | Method and apparatus for virtual digital subtraction angiography |
| US20050165292A1 (en) * | 2002-04-04 | 2005-07-28 | Simon David A. | Method and apparatus for virtual digital subtraction angiography |
| US9642514B2 (en) | 2002-04-17 | 2017-05-09 | Covidien Lp | Endoscope structures and techniques for navigating to a target in a branched structure |
| US10743748B2 (en) | 2002-04-17 | 2020-08-18 | Covidien Lp | Endoscope structures and techniques for navigating to a target in branched structure |
| US8696548B2 (en) | 2002-04-17 | 2014-04-15 | Covidien Lp | Endoscope structures and techniques for navigating to a target in branched structure |
| US8696685B2 (en) | 2002-04-17 | 2014-04-15 | Covidien Lp | Endoscope structures and techniques for navigating to a target in branched structure |
| US8401616B2 (en) | 2002-11-19 | 2013-03-19 | Medtronic Navigation, Inc. | Navigation system for cardiac therapies |
| US8060185B2 (en) | 2002-11-19 | 2011-11-15 | Medtronic Navigation, Inc. | Navigation system for cardiac therapies |
| US20040097806A1 (en) * | 2002-11-19 | 2004-05-20 | Mark Hunter | Navigation system for cardiac therapies |
| US20100210938A1 (en) * | 2002-11-19 | 2010-08-19 | Medtronic Navigation, Inc | Navigation System for Cardiac Therapies |
| US7697972B2 (en) | 2002-11-19 | 2010-04-13 | Medtronic Navigation, Inc. | Navigation system for cardiac therapies |
| US20040097805A1 (en) * | 2002-11-19 | 2004-05-20 | Laurent Verard | Navigation system for cardiac therapies |
| US8046052B2 (en) | 2002-11-19 | 2011-10-25 | Medtronic Navigation, Inc. | Navigation system for cardiac therapies |
| US20100022873A1 (en) * | 2002-11-19 | 2010-01-28 | Surgical Navigation Technologies, Inc. | Navigation System for Cardiac Therapies |
| US8467853B2 (en) | 2002-11-19 | 2013-06-18 | Medtronic Navigation, Inc. | Navigation system for cardiac therapies |
| US7660623B2 (en) | 2003-01-30 | 2010-02-09 | Medtronic Navigation, Inc. | Six degree of freedom alignment display for medical procedures |
| US9867721B2 (en) | 2003-01-30 | 2018-01-16 | Medtronic Navigation, Inc. | Method and apparatus for post-operative tuning of a spinal implant |
| US7974677B2 (en) | 2003-01-30 | 2011-07-05 | Medtronic Navigation, Inc. | Method and apparatus for preplanning a surgical procedure |
| US20040171924A1 (en) * | 2003-01-30 | 2004-09-02 | Mire David A. | Method and apparatus for preplanning a surgical procedure |
| US20090234217A1 (en) * | 2003-01-30 | 2009-09-17 | Surgical Navigation Technologies, Inc. | Method And Apparatus For Preplanning A Surgical Procedure |
| US20040152972A1 (en) * | 2003-01-30 | 2004-08-05 | Mark Hunter | Method and apparatus for post-operative tuning of a spinal implant |
| US11707363B2 (en) | 2003-01-30 | 2023-07-25 | Medtronic Navigation, Inc. | Method and apparatus for post-operative tuning of a spinal implant |
| US11684491B2 (en) | 2003-01-30 | 2023-06-27 | Medtronic Navigation, Inc. | Method and apparatus for post-operative tuning of a spinal implant |
| US20040215071A1 (en) * | 2003-04-25 | 2004-10-28 | Frank Kevin J. | Method and apparatus for performing 2D to 3D registration |
| US7925328B2 (en) | 2003-08-28 | 2011-04-12 | Medtronic Navigation, Inc. | Method and apparatus for performing stereotactic surgery |
| US20080097195A1 (en) * | 2003-08-28 | 2008-04-24 | Surgical Navigation Technologies, Inc. | Method and apparatus for performing stereotactic surgery |
| US9089261B2 (en) | 2003-09-15 | 2015-07-28 | Covidien Lp | System of accessories for use with bronchoscopes |
| US10383509B2 (en) | 2003-09-15 | 2019-08-20 | Covidien Lp | System of accessories for use with bronchoscopes |
| US8663088B2 (en) | 2003-09-15 | 2014-03-04 | Covidien Lp | System of accessories for use with bronchoscopes |
| US8706185B2 (en) | 2003-10-16 | 2014-04-22 | Medtronic Navigation, Inc. | Method and apparatus for surgical navigation of a multiple piece construct for implantation |
| US7835778B2 (en) | 2003-10-16 | 2010-11-16 | Medtronic Navigation, Inc. | Method and apparatus for surgical navigation of a multiple piece construct for implantation |
| US20050085714A1 (en) * | 2003-10-16 | 2005-04-21 | Foley Kevin T. | Method and apparatus for surgical navigation of a multiple piece construct for implantation |
| US8359730B2 (en) | 2003-10-17 | 2013-01-29 | Medtronic Navigation, Inc. | Method of forming an electromagnetic sensing coil in a medical instrument |
| US20050085720A1 (en) * | 2003-10-17 | 2005-04-21 | Jascob Bradley A. | Method and apparatus for surgical navigation |
| US20060025677A1 (en) * | 2003-10-17 | 2006-02-02 | Verard Laurent G | Method and apparatus for surgical navigation |
| US8271069B2 (en) * | 2003-10-17 | 2012-09-18 | Medtronic Navigation, Inc. | Method and apparatus for surgical navigation |
| US7840253B2 (en) | 2003-10-17 | 2010-11-23 | Medtronic Navigation, Inc. | Method and apparatus for surgical navigation |
| US20100274124A1 (en) * | 2003-10-17 | 2010-10-28 | Medtronic Navigation, Inc. | Method and Apparatus for Surgical Navigation |
| US7971341B2 (en) | 2003-10-17 | 2011-07-05 | Medtronic Navigation, Inc. | Method of forming an electromagnetic sensing coil in a medical instrument for a surgical navigation system |
| US20080171937A1 (en) * | 2003-10-17 | 2008-07-17 | Surgical Navigation Technologies, Inc | Method And Apparatus For Surgical Navigation |
| US7751865B2 (en) | 2003-10-17 | 2010-07-06 | Medtronic Navigation, Inc. | Method and apparatus for surgical navigation |
| US20080172069A1 (en) * | 2003-10-17 | 2008-07-17 | Surgical Navigation Technologies, Inc | Method And Apparatus For Surgical Navigation |
| US8239001B2 (en) | 2003-10-17 | 2012-08-07 | Medtronic Navigation, Inc. | Method and apparatus for surgical navigation |
| US8549732B2 (en) | 2003-10-17 | 2013-10-08 | Medtronic Navigation, Inc. | Method of forming an electromagnetic sensing coil in a medical instrument |
| US7818044B2 (en) | 2003-10-17 | 2010-10-19 | Medtronic Navigation, Inc. | Method and apparatus for surgical navigation |
| US20060084867A1 (en) * | 2003-10-17 | 2006-04-20 | Tremblay Brian M | Method and apparatus for surgical navigation |
| US8764725B2 (en) | 2004-02-09 | 2014-07-01 | Covidien Lp | Directional anchoring mechanism, method and applications thereof |
| US10582879B2 (en) | 2004-02-17 | 2020-03-10 | Philips Electronics Ltd | Method and apparatus for registration, verification and referencing of internal organs |
| US7998062B2 (en) | 2004-03-29 | 2011-08-16 | Superdimension, Ltd. | Endoscope structures and techniques for navigating to a target in branched structure |
| US9055881B2 (en) | 2004-04-26 | 2015-06-16 | Super Dimension Ltd. | System and method for image-based alignment of an endoscope |
| US10321803B2 (en) | 2004-04-26 | 2019-06-18 | Covidien Lp | System and method for image-based alignment of an endoscope |
| US20080262297A1 (en) * | 2004-04-26 | 2008-10-23 | Super Dimension Ltd. | System and Method for Image-Based Alignment of an Endoscope |
| US7953471B2 (en) | 2004-05-03 | 2011-05-31 | Medtronic Navigation, Inc. | Method and apparatus for implantation between two vertebral bodies |
| US20050245817A1 (en) * | 2004-05-03 | 2005-11-03 | Clayton John B | Method and apparatus for implantation between two vertebral bodies |
| US8406845B2 (en) * | 2004-09-01 | 2013-03-26 | University Of Tennessee Research Foundation | Method and apparatus for imaging tracking |
| US20060058645A1 (en) * | 2004-09-01 | 2006-03-16 | Komistek Richard D | Method and apparatus for imaging tracking |
| US20060094958A1 (en) * | 2004-10-28 | 2006-05-04 | Marquart Joel G | Method and apparatus for calibrating non-linear instruments |
| US20080071215A1 (en) * | 2004-11-05 | 2008-03-20 | Traxtal Technologies Inc. | Access System |
| US7722565B2 (en) | 2004-11-05 | 2010-05-25 | Traxtal, Inc. | Access system |
| US20060122497A1 (en) * | 2004-11-12 | 2006-06-08 | Glossop Neil D | Device and method for ensuring the accuracy of a tracking device in a volume |
| US20060173269A1 (en) * | 2004-11-12 | 2006-08-03 | Glossop Neil D | Integrated skin-mounted multifunction device for use in image-guided surgery |
| US7751868B2 (en) | 2004-11-12 | 2010-07-06 | Philips Electronics Ltd | Integrated skin-mounted multifunction device for use in image-guided surgery |
| US7805269B2 (en) | 2004-11-12 | 2010-09-28 | Philips Electronics Ltd | Device and method for ensuring the accuracy of a tracking device in a volume |
| US7840254B2 (en) | 2005-01-18 | 2010-11-23 | Philips Electronics Ltd | Electromagnetically tracked K-wire device |
| US20060173291A1 (en) * | 2005-01-18 | 2006-08-03 | Glossop Neil D | Electromagnetically tracked K-wire device |
| US8611983B2 (en) | 2005-01-18 | 2013-12-17 | Philips Electronics Ltd | Method and apparatus for guiding an instrument to a target in the lung |
| US20060170417A1 (en) * | 2005-02-02 | 2006-08-03 | Rodgers Allan G | Distributed array magnetic tracking |
| US20060199159A1 (en) * | 2005-03-01 | 2006-09-07 | Neuronetics, Inc. | Head phantom for simulating the patient response to magnetic stimulation |
| US20070167787A1 (en) * | 2005-06-21 | 2007-07-19 | Glossop Neil D | Device and method for a trackable ultrasound |
| US20070032723A1 (en) * | 2005-06-21 | 2007-02-08 | Glossop Neil D | System, method and apparatus for navigated therapy and diagnosis |
| US9398892B2 (en) | 2005-06-21 | 2016-07-26 | Koninklijke Philips N.V. | Device and method for a trackable ultrasound |
| US8632461B2 (en) | 2005-06-21 | 2014-01-21 | Koninklijke Philips N.V. | System, method and apparatus for navigated therapy and diagnosis |
| WO2007025081A3 (en) * | 2005-08-24 | 2007-12-06 | Traxtal Inc | System, method and devices for navigated flexible endoscopy |
| US9661991B2 (en) | 2005-08-24 | 2017-05-30 | Koninklijke Philips N.V. | System, method and devices for navigated flexible endoscopy |
| US20070055128A1 (en) * | 2005-08-24 | 2007-03-08 | Glossop Neil D | System, method and devices for navigated flexible endoscopy |
| US8547248B2 (en) | 2005-09-01 | 2013-10-01 | Proteus Digital Health, Inc. | Implantable zero-wire communications system |
| US7835784B2 (en) | 2005-09-21 | 2010-11-16 | Medtronic Navigation, Inc. | Method and apparatus for positioning a reference frame |
| US20070066887A1 (en) * | 2005-09-21 | 2007-03-22 | Mire David A | Method and apparatus for positioning a reference frame |
| US8467851B2 (en) | 2005-09-21 | 2013-06-18 | Medtronic Navigation, Inc. | Method and apparatus for positioning a reference frame |
| US8494805B2 (en) | 2005-11-28 | 2013-07-23 | Orthosensor | Method and system for assessing orthopedic alignment using tracking sensors |
| US20100204955A1 (en) * | 2005-11-28 | 2010-08-12 | Martin Roche | Method and system for positional measurement using ultrasonic sensing |
| US8000926B2 (en) | 2005-11-28 | 2011-08-16 | Orthosensor | Method and system for positional measurement using ultrasonic sensing |
| US8098544B2 (en) | 2005-11-29 | 2012-01-17 | Orthosensor, Inc. | Method and system for enhancing accuracy in ultrasonic alignment |
| US8270253B1 (en) | 2005-11-29 | 2012-09-18 | Orthosensor, Inc. | Method and system for ultrasonic measurement and alignment |
| US20100204575A1 (en) * | 2005-11-29 | 2010-08-12 | Martin Roche | Method and system for enhancing accuracy in ultrasonic alignment |
| US20110060220A1 (en) * | 2005-12-01 | 2011-03-10 | Martin Roche | Virtual mapping of an anatomical pivot point and alignment therewith |
| US20110032184A1 (en) * | 2005-12-01 | 2011-02-10 | Martin Roche | Orthopedic method and system for mapping an anatomical pivot point |
| US8814810B2 (en) | 2005-12-01 | 2014-08-26 | Orthosensor Inc. | Orthopedic method and system for mapping an anatomical pivot point |
| US8864686B2 (en) | 2005-12-01 | 2014-10-21 | Orthosensor Inc. | Virtual mapping of an anatomical pivot point and alignment therewith |
| US9168102B2 (en) | 2006-01-18 | 2015-10-27 | Medtronic Navigation, Inc. | Method and apparatus for providing a container to a sterile environment |
| US10597178B2 (en) | 2006-01-18 | 2020-03-24 | Medtronic Navigation, Inc. | Method and apparatus for providing a container to a sterile environment |
| US20070166188A1 (en) * | 2006-01-18 | 2007-07-19 | Eric Ryterski | Method and apparatus for providing a container to a sterile environment |
| US8112292B2 (en) | 2006-04-21 | 2012-02-07 | Medtronic Navigation, Inc. | Method and apparatus for optimizing a therapy |
| US20070249911A1 (en) * | 2006-04-21 | 2007-10-25 | Simon David A | Method and apparatus for optimizing a therapy |
| WO2009008894A2 (en) * | 2006-08-22 | 2009-01-15 | Dimensions Imaging | System and method for determining absolute position using a multiple wavelength signal |
| US9642571B2 (en) | 2006-08-24 | 2017-05-09 | Orthosensor Inc | System and method for sensorized user interface |
| US8421642B1 (en) | 2006-08-24 | 2013-04-16 | Navisense | System and method for sensorized user interface |
| US20080058630A1 (en) * | 2006-09-01 | 2008-03-06 | Robertson Timothy L | Simultaneous blood flow and hematocrit sensor |
| US8172762B2 (en) | 2006-09-01 | 2012-05-08 | Proteus Biomedical, Inc. | Simultaneous blood flow and hematocrit sensor |
| US8638296B1 (en) | 2006-09-05 | 2014-01-28 | Jason McIntosh | Method and machine for navigation system calibration |
| US20080081982A1 (en) * | 2006-09-29 | 2008-04-03 | Medtronic, Inc. | Method And Apparatus For Optimizing A Computer Assisted Surgical Procedure |
| US9597154B2 (en) | 2006-09-29 | 2017-03-21 | Medtronic, Inc. | Method and apparatus for optimizing a computer assisted surgical procedure |
| US8660635B2 (en) | 2006-09-29 | 2014-02-25 | Medtronic, Inc. | Method and apparatus for optimizing a computer assisted surgical procedure |
| US20080119712A1 (en) * | 2006-11-20 | 2008-05-22 | General Electric Company | Systems and Methods for Automated Image Registration |
| US11771502B2 (en) | 2007-06-15 | 2023-10-03 | Orthosoft Ulc | Computer-assisted surgery system and method |
| US11116577B2 (en) * | 2007-06-15 | 2021-09-14 | Orthosoft Ulc | Computer-assisted surgery system and method |
| US20080312529A1 (en) * | 2007-06-15 | 2008-12-18 | Louis-Philippe Amiot | Computer-assisted surgery system and method |
| US9532848B2 (en) * | 2007-06-15 | 2017-01-03 | Othosoft, Inc. | Computer-assisted surgery system and method |
| US10980400B2 (en) | 2007-09-27 | 2021-04-20 | Covidien Lp | Bronchoscope adapter and method |
| US10390686B2 (en) | 2007-09-27 | 2019-08-27 | Covidien Lp | Bronchoscope adapter and method |
| US8905920B2 (en) | 2007-09-27 | 2014-12-09 | Covidien Lp | Bronchoscope adapter and method |
| US9986895B2 (en) | 2007-09-27 | 2018-06-05 | Covidien Lp | Bronchoscope adapter and method |
| US9668639B2 (en) | 2007-09-27 | 2017-06-06 | Covidien Lp | Bronchoscope adapter and method |
| US9189083B2 (en) | 2008-03-18 | 2015-11-17 | Orthosensor Inc. | Method and system for media presentation during operative workflow |
| US9575140B2 (en) | 2008-04-03 | 2017-02-21 | Covidien Lp | Magnetic interference detection system and method |
| US11074702B2 (en) | 2008-06-03 | 2021-07-27 | Covidien Lp | Feature-based registration method |
| US11783498B2 (en) | 2008-06-03 | 2023-10-10 | Covidien Lp | Feature-based registration method |
| US9117258B2 (en) | 2008-06-03 | 2015-08-25 | Covidien Lp | Feature-based registration method |
| US9659374B2 (en) | 2008-06-03 | 2017-05-23 | Covidien Lp | Feature-based registration method |
| US10096126B2 (en) | 2008-06-03 | 2018-10-09 | Covidien Lp | Feature-based registration method |
| US8473032B2 (en) | 2008-06-03 | 2013-06-25 | Superdimension, Ltd. | Feature-based registration method |
| US8467589B2 (en) | 2008-06-06 | 2013-06-18 | Covidien Lp | Hybrid registration method |
| US11931141B2 (en) | 2008-06-06 | 2024-03-19 | Covidien Lp | Hybrid registration method |
| US9271803B2 (en) | 2008-06-06 | 2016-03-01 | Covidien Lp | Hybrid registration method |
| US10674936B2 (en) | 2008-06-06 | 2020-06-09 | Covidien Lp | Hybrid registration method |
| US10478092B2 (en) | 2008-06-06 | 2019-11-19 | Covidien Lp | Hybrid registration method |
| US8452068B2 (en) | 2008-06-06 | 2013-05-28 | Covidien Lp | Hybrid registration method |
| US10285623B2 (en) | 2008-06-06 | 2019-05-14 | Covidien Lp | Hybrid registration method |
| US11241164B2 (en) | 2008-07-10 | 2022-02-08 | Covidien Lp | Integrated multi-functional endoscopic tool |
| US11234611B2 (en) | 2008-07-10 | 2022-02-01 | Covidien Lp | Integrated multi-functional endoscopic tool |
| US10912487B2 (en) | 2008-07-10 | 2021-02-09 | Covidien Lp | Integrated multi-function endoscopic tool |
| US10070801B2 (en) | 2008-07-10 | 2018-09-11 | Covidien Lp | Integrated multi-functional endoscopic tool |
| US8932207B2 (en) | 2008-07-10 | 2015-01-13 | Covidien Lp | Integrated multi-functional endoscopic tool |
| US8165658B2 (en) | 2008-09-26 | 2012-04-24 | Medtronic, Inc. | Method and apparatus for positioning a guide relative to a base |
| US8175681B2 (en) | 2008-12-16 | 2012-05-08 | Medtronic Navigation Inc. | Combination of electromagnetic and electropotential localization |
| US8731641B2 (en) | 2008-12-16 | 2014-05-20 | Medtronic Navigation, Inc. | Combination of electromagnetic and electropotential localization |
| US10154798B2 (en) | 2009-04-08 | 2018-12-18 | Covidien Lp | Locatable catheter |
| US8611984B2 (en) | 2009-04-08 | 2013-12-17 | Covidien Lp | Locatable catheter |
| US9113813B2 (en) | 2009-04-08 | 2015-08-25 | Covidien Lp | Locatable catheter |
| US20110207997A1 (en) * | 2009-04-08 | 2011-08-25 | Superdimension, Ltd. | Locatable Catheter |
| US20120136626A1 (en) * | 2009-05-18 | 2012-05-31 | Dirk Mucha | Method for generating position data of an instrument |
| US10398512B2 (en) * | 2009-05-18 | 2019-09-03 | Dirk Mucha | Method for generating position data of an instrument |
| US8494613B2 (en) | 2009-08-31 | 2013-07-23 | Medtronic, Inc. | Combination localization system |
| US8494614B2 (en) | 2009-08-31 | 2013-07-23 | Regents Of The University Of Minnesota | Combination localization system |
| US9011448B2 (en) | 2009-12-31 | 2015-04-21 | Orthosensor Inc. | Orthopedic navigation system with sensorized devices |
| US9452023B2 (en) | 2009-12-31 | 2016-09-27 | Orthosensor Inc. | Operating room surgical field device and method therefore |
| US20110160738A1 (en) * | 2009-12-31 | 2011-06-30 | Orthosensor | Operating room surgical field device and method therefore |
| US20110160572A1 (en) * | 2009-12-31 | 2011-06-30 | Orthosensor | Disposable wand and sensor for orthopedic alignment |
| US20110160583A1 (en) * | 2009-12-31 | 2011-06-30 | Orthosensor | Orthopedic Navigation System with Sensorized Devices |
| US9452022B2 (en) | 2009-12-31 | 2016-09-27 | Orthosensor Inc | Disposable wand and sensor for orthopedic alignment |
| US10582834B2 (en) | 2010-06-15 | 2020-03-10 | Covidien Lp | Locatable expandable working channel and method |
| US8892186B2 (en) * | 2010-09-20 | 2014-11-18 | Siemens Aktiengesellschaft | Method and system for detection and tracking of coronary sinus catheter electrodes in fluoroscopic images |
| US20120070046A1 (en) * | 2010-09-20 | 2012-03-22 | Siemens Corporation | Method and System for Detection and Tracking of Coronary Sinus Catheter Electrodes in Fluoroscopic Images |
| US8613714B2 (en) | 2010-10-05 | 2013-12-24 | Cerevast Therapeutics, Inc. | Non-invasive transcranial ultrasound apparatus |
| US8603014B2 (en) | 2010-10-05 | 2013-12-10 | Cerevast Therapeutics, Inc. | Hands-free operator-independent transcranial ultrasound apparatus and methods |
| US9220467B2 (en) * | 2011-09-19 | 2015-12-29 | Siemens Aktiengesellschaft | Method and system for tracking catheters in 2D X-ray fluoroscopy using a graphics processing unit |
| US20130072788A1 (en) * | 2011-09-19 | 2013-03-21 | Siemens Aktiengesellschaft | Method and System for Tracking Catheters in 2D X-Ray Fluoroscopy Using a Graphics Processing Unit |
| US10575906B2 (en) | 2012-09-26 | 2020-03-03 | Stryker Corporation | Navigation system and method for tracking objects using optical and non-optical sensors |
| US11529198B2 (en) | 2012-09-26 | 2022-12-20 | Stryker Corporation | Optical and non-optical sensor tracking of objects for a robotic cutting system |
| US9271804B2 (en) | 2012-09-26 | 2016-03-01 | Stryker Corporation | Method for tracking objects using optical and non-optical sensors |
| US9687307B2 (en) | 2012-09-26 | 2017-06-27 | Stryker Corporation | Navigation system and method for tracking objects using optical and non-optical sensors |
| US9008757B2 (en) | 2012-09-26 | 2015-04-14 | Stryker Corporation | Navigation system including optical and non-optical sensors |
| US11357574B2 (en) | 2013-10-31 | 2022-06-14 | Intersect ENT International GmbH | Surgical instrument and method for detecting the position of a surgical instrument |
| US10952593B2 (en) | 2014-06-10 | 2021-03-23 | Covidien Lp | Bronchoscope adapter |
| US10426555B2 (en) | 2015-06-03 | 2019-10-01 | Covidien Lp | Medical instrument with sensor for use in a system and method for electromagnetic navigation |
| US11006914B2 (en) | 2015-10-28 | 2021-05-18 | Medtronic Navigation, Inc. | Apparatus and method for maintaining image quality while minimizing x-ray dosage of a patient |
| US11801024B2 (en) | 2015-10-28 | 2023-10-31 | Medtronic Navigation, Inc. | Apparatus and method for maintaining image quality while minimizing x-ray dosage of a patient |
| US10478254B2 (en) | 2016-05-16 | 2019-11-19 | Covidien Lp | System and method to access lung tissue |
| US11786317B2 (en) | 2016-05-16 | 2023-10-17 | Covidien Lp | System and method to access lung tissue |
| US11160617B2 (en) | 2016-05-16 | 2021-11-02 | Covidien Lp | System and method to access lung tissue |
| US10722311B2 (en) | 2016-10-28 | 2020-07-28 | Covidien Lp | System and method for identifying a location and/or an orientation of an electromagnetic sensor based on a map |
| US11786314B2 (en) | 2016-10-28 | 2023-10-17 | Covidien Lp | System for calibrating an electromagnetic navigation system |
| US10418705B2 (en) | 2016-10-28 | 2019-09-17 | Covidien Lp | Electromagnetic navigation antenna assembly and electromagnetic navigation system including the same |
| US10792106B2 (en) | 2016-10-28 | 2020-10-06 | Covidien Lp | System for calibrating an electromagnetic navigation system |
| US10446931B2 (en) | 2016-10-28 | 2019-10-15 | Covidien Lp | Electromagnetic navigation antenna assembly and electromagnetic navigation system including the same |
| US10517505B2 (en) | 2016-10-28 | 2019-12-31 | Covidien Lp | Systems, methods, and computer-readable media for optimizing an electromagnetic navigation system |
| US10751126B2 (en) | 2016-10-28 | 2020-08-25 | Covidien Lp | System and method for generating a map for electromagnetic navigation |
| US11672604B2 (en) | 2016-10-28 | 2023-06-13 | Covidien Lp | System and method for generating a map for electromagnetic navigation |
| US10615500B2 (en) | 2016-10-28 | 2020-04-07 | Covidien Lp | System and method for designing electromagnetic navigation antenna assemblies |
| US10638952B2 (en) | 2016-10-28 | 2020-05-05 | Covidien Lp | Methods, systems, and computer-readable media for calibrating an electromagnetic navigation system |
| US11759264B2 (en) | 2016-10-28 | 2023-09-19 | Covidien Lp | System and method for identifying a location and/or an orientation of an electromagnetic sensor based on a map |
| US11164679B2 (en) | 2017-06-20 | 2021-11-02 | Advinow, Inc. | Systems and methods for intelligent patient interface exam station |
| US11219489B2 (en) | 2017-10-31 | 2022-01-11 | Covidien Lp | Devices and systems for providing sensors in parallel with medical tools |
| US11348688B2 (en) * | 2018-03-06 | 2022-05-31 | Advinow, Inc. | Systems and methods for audio medical instrument patient measurements |
| US11430139B2 (en) | 2019-04-03 | 2022-08-30 | Intersect ENT International GmbH | Registration method and setup |
| WO2021074326A1 (en) * | 2019-10-15 | 2021-04-22 | Fiagon Ag Medical Technologies | Automatic medical instrument identification |
| US20220287635A1 (en) * | 2021-03-10 | 2022-09-15 | Livivos Inc. | Systems and methods for non-invasive fat composition measurement in an organ |
| US11896392B2 (en) * | 2021-03-10 | 2024-02-13 | Livivos Inc. | Systems and methods for non-invasive fat composition measurement in an organ |
Also Published As
| Publication number | Publication date |
|---|---|
| JPH11318937A (en) | 1999-11-24 |
| US5676673A (en) | 1997-10-14 |
| EP0951874A2 (en) | 1999-10-27 |
| US6694167B1 (en) | 2004-02-17 |
| DE69531994D1 (en) | 2003-11-27 |
| US5803089A (en) | 1998-09-08 |
| US5873822A (en) | 1999-02-23 |
| US20060036151A1 (en) | 2006-02-16 |
| EP0951874A3 (en) | 2000-06-14 |
| DE69531994T2 (en) | 2004-07-22 |
| US6738656B1 (en) | 2004-05-18 |
| US6341231B1 (en) | 2002-01-22 |
| US6687531B1 (en) | 2004-02-03 |
| US5800352A (en) | 1998-09-01 |
| US20070083107A1 (en) | 2007-04-12 |
| US8473026B2 (en) | 2013-06-25 |
| JP3325533B2 (en) | 2002-09-17 |
| ATE252349T1 (en) | 2003-11-15 |
| US6175756B1 (en) | 2001-01-16 |
Similar Documents
| Publication | Publication Date | Title |
|---|---|---|
| US6175756B1 (en) | Position tracking and imaging system for use in medical applications | |
| EP0782413B1 (en) | Position tracking system for use in medical applications using a reference unit secured to a patient's head | |
| EP1380266B1 (en) | Position tracking and imaging system for use in medical applications | |
| US9398892B2 (en) | Device and method for a trackable ultrasound | |
| US7060075B2 (en) | Distal targeting of locking screws in intramedullary nails | |
| US6167292A (en) | Registering method and apparatus for robotic surgery, and a registering device constituting an application thereof | |
| US7535411B2 (en) | System and method for detecting drifts in calibrated tracking systems | |
| JP3135068B2 (en) | Position tracking and image generation system for medical applications using a reference unit fixed to the patient's head | |
| IL126491A (en) | X-ray guided surgical location system with extended mapping volume | |
| EP1259160A2 (en) | Apparatus and methods for medical interventions | |
| JPH05119136A (en) | Measuring method for position and direction of detection coil of squid sensor |
Legal Events
| Date | Code | Title | Description |
|---|---|---|---|
| AS | Assignment |
Owner name: GE MEDICAL SYSTEMS GLOBAL TECHNOLOGY COMPANY, LLC, Free format text: ASSIGNMENT OF ASSIGNORS INTEREST;ASSIGNOR:OEC MEDICAL SYSTEMS, INC.;REEL/FRAME:014567/0262 Effective date: 20030925 |
|
| AS | Assignment |
Owner name: VISUALIZATION TECHNOLOGY, INC., MASSACHUSETTS Free format text: MERGER;ASSIGNOR:EMERALD MERGER CORPORATION;REEL/FRAME:016647/0028 Effective date: 20020212 Owner name: OEC MEDICAL SYSTEMS, INC., UTAH Free format text: MERGER;ASSIGNOR:GE MEDICAL SYSTEMS NAVIGATION AND VISUALIZATION;REEL/FRAME:016648/0327 Effective date: 20020927 Owner name: GE MEDICAL SYSTEMS NAVIGATION AND VISULIZATION, DE Free format text: CHANGE OF NAME;ASSIGNOR:VISUALIZATION TECHNOLOGY, INC.;REEL/FRAME:016648/0321 Effective date: 20020212 |
|
| STCB | Information on status: application discontinuation |
Free format text: ABANDONED -- AFTER EXAMINER'S ANSWER OR BOARD OF APPEALS DECISION |